It is not uncommon for people with type 1 diabetes to have reservations about living alone.
Usually the main concerns for people with type 1 diabetes living on their own are over what happens if short term complications, such as severe hypos or ketoacidosis, occur.
The following guide has been put together to help ease these concerns.
Nocturnal hypos
Hypos at night can be a particular worry for those of us with type 1 diabetes living on our ow, or away from home.
To minimise the risk of hypos, it’s important to get the basics right:
- Always test before going to bed
- Test as soon as you wake up whenever possible
- Always have sweets, ideally glucose tablets, beside your bed
- Ensure you take your long acting (basal) insulin at the correct times
- Aim to maintai, where possible, a regular schedule of when you eat and when you go to bed
If you have taken exercise, or alcohol earlier in the day, consider setting an alarm during the night to test your blood glucose levels.
Setting an alarm during the night is also advisable if you are otherwise unsure of how your blood glucose levels may behave overnight This may be the case during or following periods of illness or if you have recently made changes to your diet, activity levels or insulin doses
If you are worried about hypos during the night, it may be a good idea to ask a friend or relative to call you or otherwise check on you in the morning.
Hypo unawareness
If you have lost your awareness of hypoglycemia (being unable to sense when you are hypo), living alone could increase the danger you face as no-one will be there to help you.
If you are at significant risk, your health team may provide you with more advanced technology for managing your diabetes or other methods of support.
Advanced support for preventing severe hypos
If you are having regular severe hypos, you should consult your diabetes health team. They can help you with ensuring you have the right insulin doses and may be able to help towards providing you with one of the following methods of support.
Insulin pumps allow people to deliver different rates of background (basal) insulin at different times of day and therefore provide more control for preventing hypos over night.
Continuous glucose monitors are not routinely provided on the NHS but may be made available to people with a specific clinical need for them, such as people having great difficulty preventing hypos during the night or day.
Hypo alert dogs are dogs that are specially trained to alert their owner when they are suffering from medical problems such as hypoglycemia or ketoacidosis. In certain cases, it may be possible to have your own dog trained
Ketoacidosis
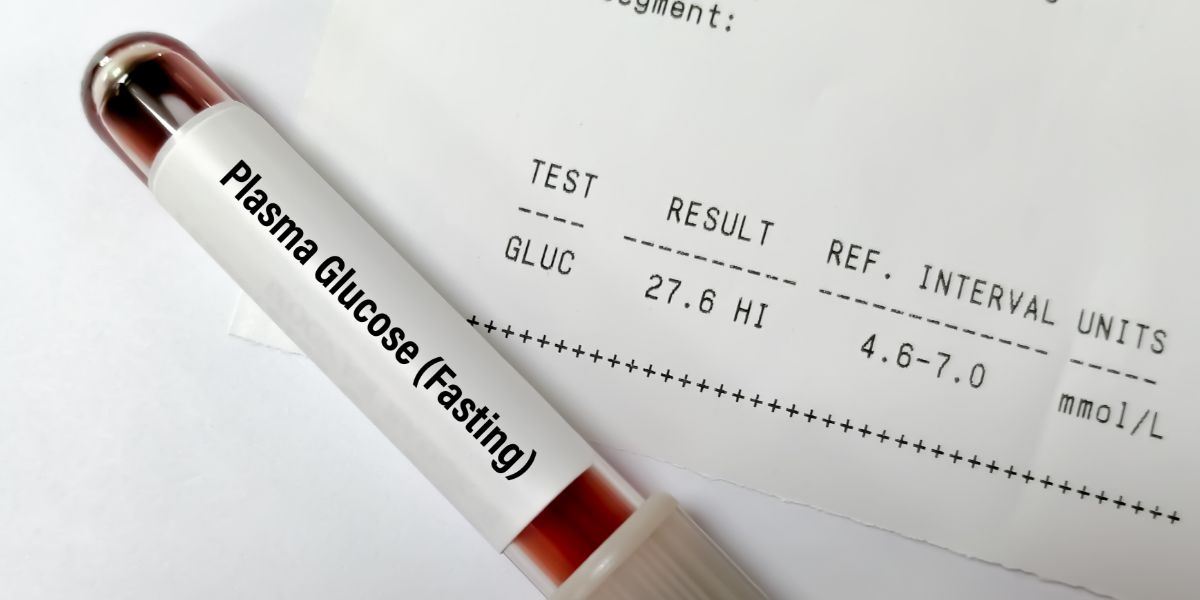
Diabetic ketoacidosis (DKA) is a serious short term complication that occurs if the body has too little insulin for an extended period of time.
Ketoacidosis may be more likely to occur under the following conditions:
- During periods of illness
- During stressful times, if this causes insulin doses to be forgotten
- If there is a problem with your insulin, insulin pen or insulin pump
Ketoacidosis can usually be prevented by ensuring you don’t miss or delay insulin injections or insulin pump doses, and by taking regular blood glucose tests. Ketone testing can also help to minimise risks of suffering ketoacidosis.
Illness
Going through periods of illness can place extra demands on diabetes management. It is common for blood glucose levels to rise in response to illness and this may require increased insulin doses.
In addition, illness may cause you to feel more lethargic than usual and could even make symptoms of high or low blood sugar levels harder to spot
If you become ill, it is important to prioritise your diabetes management and ensure you take all the injections you need to and continue regularly taking blood glucose tests, particularly before any time you go to sleep, whether during the night or day.
If your illness makes it significantly harder for you to control your diabetes, you may want to consider staying with family or friends until you recover. Alternatively, you may want to ask someone (a close friend or relative) to call or otherwise check on you whilst you’re ill.
Alcohol
Alcohol affects the body in a number of ways that can increase the risk of too high or too low blood sugar levels.
On the one hand, alcohol can make people more likely to forget to do insulin injections or blood tests and it can also the ability to make accurate judgements, which could affect insulin doses or carbohydrate intake
It also has the effect of inhibiting the liver from releasing glucose into the blood. This is why alcohol is associated lower blood glucose levels, particularly during the night. This can be particularly dangerous during sleep as alcohol may prevent the liver from raising blood glucose in response to a hypo, an action it can usually take if a hypo is not treated quickly.
Ideally, it’s best to not to consume larger amounts of alcohol. Another strong danger is if strenuous exercise within the last day or two is followed by alcohol as these factors can each add to the risks of suffering a dangerous hypo.
If you have been drinking, make sure you take your basal insulin at the right time to decrease the risk of ketoacidosis and take carbohydrate before bed to prevent hypos occurring over night.
- Read more about alcohol and preventing hypos