- Messages
- 26
- Type of diabetes
- Type 2
- Treatment type
- Non-insulin injectable medication (incretin mimetics)
Background Info:
I'm not type I, but had an extreme adverse reaction to metformin, lactic acidosis. 1.8mg daily Victoza injection worked well for about a year, then levels started rising with no changes in my diet. Gliclazide was added at 30mg then 60mg per day, but had a very sporadic effect at first, working too well on some days but not at all on others, and now has no effect for the past several weeks. I went back to 30mg gliclazide one day due to running out and not being able to get the prescription refilled, and that made no difference in my blood sugar levels.
Unable to get in to see anyone to deal with this for another month, since my GP doesn't want to deal with it and there's a long wait to get referred to the specialist), I upped the gliclazide dose to the recommended official maximum of 120mg and it didn't help at all. I stopped taking it entirely 2 days ago, and it's had no impact on my blood sugar readings. Some symptoms (sporadic headache, bouts of vertigo, tremors) seem to have resolved since I stopped taking gliclazide - but these are also symptoms of my other chronic illness, so I don't know if their cessation is related to the cessation of gliclazide.
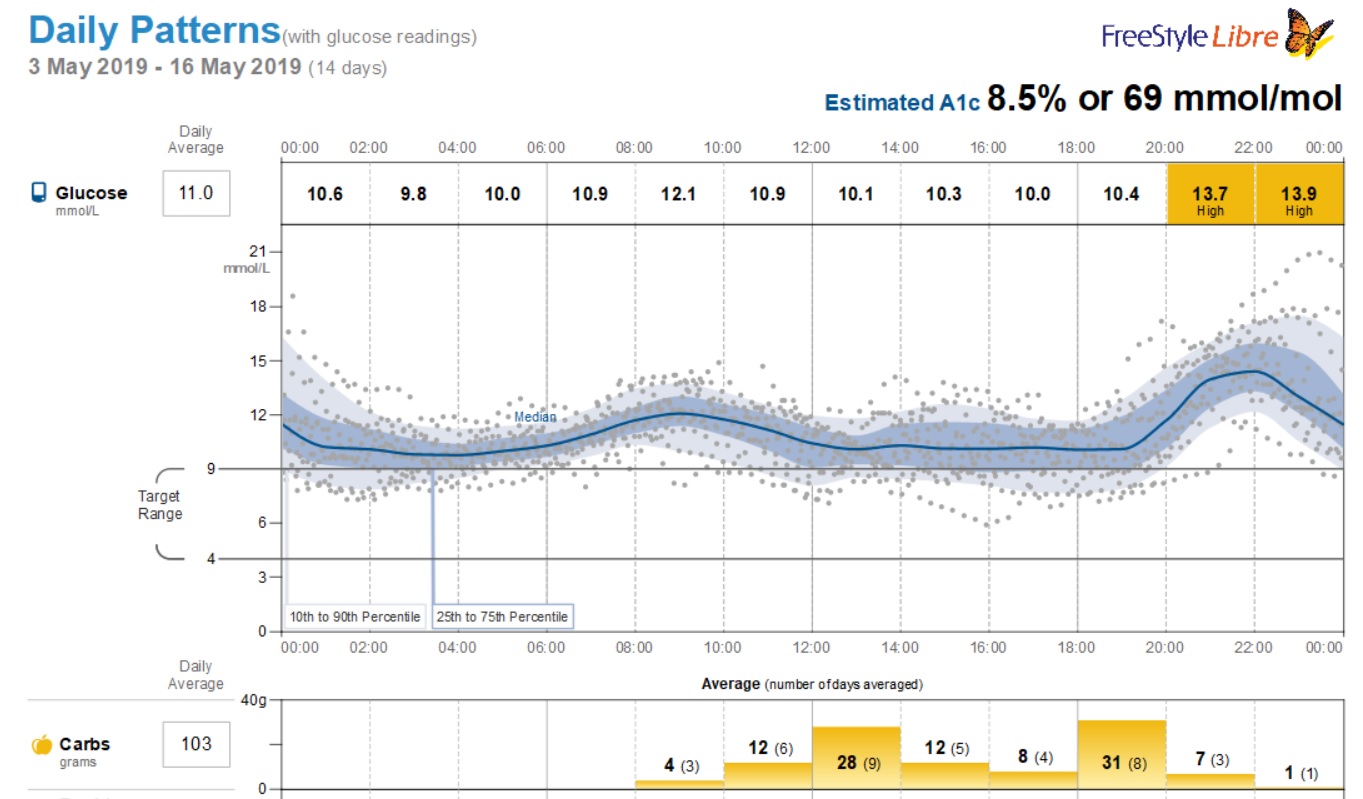
I've been using FreeStyle Libre constant monitoring for a couple months, and my average blood sugar keeps rising. It was about 10.5 (190) average for the entire day a month ago, and now it's up to 11.1 for the past week. Basically it just keeps creeping up, and it's now at the point where I'm basically hyperglycemic all day. My fasting is usually 11-14 (200-250), then goes down after a few hours of not eating any carbs. It goes up a lot after dinner typically to 14-19 (250-350. Aside from a couple hours during midday, every 10 carbs = an extra point of glucose, and it takes several hours to drop again.
Since metformin isn't an option, gliclazide isn't doing anything, and Victoza isn't helping enough, it seems like insulin is unavoidable at this point.
Question:
Are Type 2's usually started on long-acting or short-acting insulin first, when insulin is required? What's a common starting dose, and how is it calculated? I looked at a couple sites which try to explain it, but my brain couldn't process it at all :-(
Related Info:
My diabetes is secondary to a mitochondrial disease. Exercising makes me extremely ill and raises my blood sugar, presumably due to whatever it is that shuts down the rest of my body when exercising. I CANNOT EAT LOW CARB. Please do not suggest that I eat low carb: I'm sick of having it shoved down my throat here, and extremely cranky currently due to the chronic hyperglycemia, and I don't want to be forced to verbally eviscerate anyone Due to the same mitochondrial disease, cutting off a source of energy really messes me up, and leaves me completely nonfunctional.
Due to the same mitochondrial disease, cutting off a source of energy really messes me up, and leaves me completely nonfunctional.
I do limit my carbs, aiming for 100 per day. Less is nice, but hard for me to prepare because I can only sit and stand for a total of about 1 hour per day currently. Under 60-70 carbs makes me sicker. So basically I'm already eating less that half of the official recommended carbs.
A chart of my blood sugar over the past 2 weeks:
I'm not type I, but had an extreme adverse reaction to metformin, lactic acidosis. 1.8mg daily Victoza injection worked well for about a year, then levels started rising with no changes in my diet. Gliclazide was added at 30mg then 60mg per day, but had a very sporadic effect at first, working too well on some days but not at all on others, and now has no effect for the past several weeks. I went back to 30mg gliclazide one day due to running out and not being able to get the prescription refilled, and that made no difference in my blood sugar levels.
Unable to get in to see anyone to deal with this for another month, since my GP doesn't want to deal with it and there's a long wait to get referred to the specialist), I upped the gliclazide dose to the recommended official maximum of 120mg and it didn't help at all. I stopped taking it entirely 2 days ago, and it's had no impact on my blood sugar readings. Some symptoms (sporadic headache, bouts of vertigo, tremors) seem to have resolved since I stopped taking gliclazide - but these are also symptoms of my other chronic illness, so I don't know if their cessation is related to the cessation of gliclazide.
I've been using FreeStyle Libre constant monitoring for a couple months, and my average blood sugar keeps rising. It was about 10.5 (190) average for the entire day a month ago, and now it's up to 11.1 for the past week. Basically it just keeps creeping up, and it's now at the point where I'm basically hyperglycemic all day. My fasting is usually 11-14 (200-250), then goes down after a few hours of not eating any carbs. It goes up a lot after dinner typically to 14-19 (250-350. Aside from a couple hours during midday, every 10 carbs = an extra point of glucose, and it takes several hours to drop again.
Since metformin isn't an option, gliclazide isn't doing anything, and Victoza isn't helping enough, it seems like insulin is unavoidable at this point.
Question:
Are Type 2's usually started on long-acting or short-acting insulin first, when insulin is required? What's a common starting dose, and how is it calculated? I looked at a couple sites which try to explain it, but my brain couldn't process it at all :-(
Related Info:
My diabetes is secondary to a mitochondrial disease. Exercising makes me extremely ill and raises my blood sugar, presumably due to whatever it is that shuts down the rest of my body when exercising. I CANNOT EAT LOW CARB. Please do not suggest that I eat low carb: I'm sick of having it shoved down my throat here, and extremely cranky currently due to the chronic hyperglycemia, and I don't want to be forced to verbally eviscerate anyone
I do limit my carbs, aiming for 100 per day. Less is nice, but hard for me to prepare because I can only sit and stand for a total of about 1 hour per day currently. Under 60-70 carbs makes me sicker. So basically I'm already eating less that half of the official recommended carbs.
A chart of my blood sugar over the past 2 weeks:

