- Messages
- 331
- Type of diabetes
- Type 2
- Treatment type
- Diet only
What is the optimal level of a1c (blood glucose) to avoid or reduce diabetic complications?
As a newly diagnosed diabetic, the first question comes to the mind how fast I am going to get complications; or, whether keeping my BG in range, can I avoid or delay these complications; or what’s the cut point in terms of a1c or BG levels for a smooth sailing?
Well, I have been going through 10s of research study and papers recently, some as old as 20 years but then I started searching for more recent articles just to make sure I am updated on the information.
I highly recommend three books that if you have in your library, you will not need anything else to understand all the concepts about diet, metabolic disorder and diabetes and how to keep yourself healthy, or manage if you already have the metabolic disorder. These are;
Of course, reading all the research papers and diabetic journals will keep you updated and let you understand more the decades of hard-work put in the above three books.
The quick answer to why diabetic complications happen is the oxidative stress and glycation or AGEs (Advanced Glycation End-products). AGEs are happening in the human body consistently whether you are diabetic or non-diabetic, it’s a continuous process and you can not stop it. However, the level of AGEs production in your body depends upon how high and for how long your blood glucose has been high. The higher the BG and the longer they have been in a higher range, the more AGEs will be produced. If your blood sugar is mostly within the normal range 80-85 mg/dl, your AGEs production will be just normal (so basically you will age like Royals). Relationship of AGEs and complication is U-shaped. So below the normal or above the normal range, your AGEs production will be imbalanced. If you have had high BGs, you are producing more AGEs and hence you will have more complications because of glycation (excessive sugar attaching to your protein). Because this glycation mainly happens at the end points of neuron, it always affect eyes, kidneys, arteries, feet etc. It’s not as simple as it looks because there are lot more processes involved when you have more AGEs in the body that change your mitochondria and cell structure which ultimately produces calcification in arteries leading to cardiac abnormalities.
The bottom line is that more the blood sugar and for longer it stays on higher levels, you will have more AGEs and more diabetic complications. AGEs production in diabetic is 60% more than non-diabetic according to the book BloodSugar101 and that makes sense. The less AGEs you produce the better your chances are to avoid diabetic complications and that is a result of near normal sugars around the clock.
This research study from 2012 shows that the chronic complications were least below the a1c of 6%.
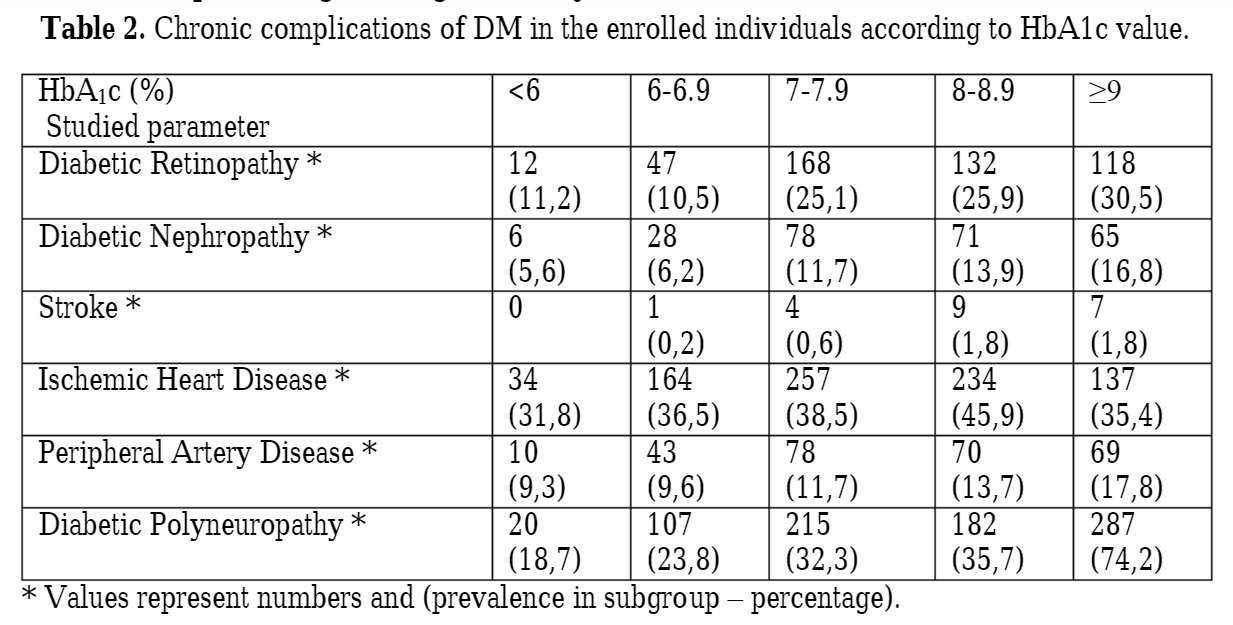
https://www.researchgate.net/public...nd_chronic_complications_in_diabetes_mellitus
This is another interesting study of a1c correlation with diabetic complications which shows that an a1c value below 6% is the safe value to target for.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3114320/
This is perhaps a more interesting study about diabetic retinopathy occurrence at different FPG and A1C levels. Its evident that prevalence of diabetic retinopathy starts when the FPG starts increasing above 5.5 mmol/l level, or when your PPG starts increasing from 9 mmol/l level, or at HBA1C level of 5.5 which seems like a cut point in this study.
Full study is here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3005450/
I could only find the reference to retinopathy complications, but in another study where the researcher correlated neuropathy and CVD as well, the threshold seems to be the same.
My conclusion (and the goals that I would set for myself) after all those months of research is as follows:
Its important to mention that AGEs are not only produced by glycation but can also be added to your body through dietary sources through what is called Maillard reaction or dAGE, however most of these dietary AGEs are excreted from the body and daily limit of dietary AGEs recommended per day is 15000 units/day (or kU/gm), which sounds very high but just a 90 gm pan fried beef steak contains over 8500 of these units.
A safe and optimal dAGE intake for the purposes of disease prevention has yet to be established. However, in animal studies, a reduction of dAGE by 50% of usual intake is associated with reduced levels of oxidative stress, less deterioration of insulin sensitivity and kidney function with age, and longer life span.
Reducing dAGE may be especially important for people with diabetes, who generate more endogenous AGEs than those without diabetes and for those with renal disease, who have impaired AGE clearance from the body
Its very interesting and a relatively new concept but if you really need to read more details about it, here is a full guide including which food has how many AGEs and what type of cooking methods increase or decrease these AGEs.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3704564/
I would be very interested to hear more about your personal experiences with your glycaemic control, number of years of diabetes and any complications that developed or reversed.
As a newly diagnosed diabetic, the first question comes to the mind how fast I am going to get complications; or, whether keeping my BG in range, can I avoid or delay these complications; or what’s the cut point in terms of a1c or BG levels for a smooth sailing?
Well, I have been going through 10s of research study and papers recently, some as old as 20 years but then I started searching for more recent articles just to make sure I am updated on the information.
I highly recommend three books that if you have in your library, you will not need anything else to understand all the concepts about diet, metabolic disorder and diabetes and how to keep yourself healthy, or manage if you already have the metabolic disorder. These are;
- Diabetic Solution by Dr. Richard K. Bernstein
- Protein Power by Dr. Michael Eades
- The Art and Science of Low Carbohydrate Living by Jeff Volek
Of course, reading all the research papers and diabetic journals will keep you updated and let you understand more the decades of hard-work put in the above three books.
The quick answer to why diabetic complications happen is the oxidative stress and glycation or AGEs (Advanced Glycation End-products). AGEs are happening in the human body consistently whether you are diabetic or non-diabetic, it’s a continuous process and you can not stop it. However, the level of AGEs production in your body depends upon how high and for how long your blood glucose has been high. The higher the BG and the longer they have been in a higher range, the more AGEs will be produced. If your blood sugar is mostly within the normal range 80-85 mg/dl, your AGEs production will be just normal (so basically you will age like Royals). Relationship of AGEs and complication is U-shaped. So below the normal or above the normal range, your AGEs production will be imbalanced. If you have had high BGs, you are producing more AGEs and hence you will have more complications because of glycation (excessive sugar attaching to your protein). Because this glycation mainly happens at the end points of neuron, it always affect eyes, kidneys, arteries, feet etc. It’s not as simple as it looks because there are lot more processes involved when you have more AGEs in the body that change your mitochondria and cell structure which ultimately produces calcification in arteries leading to cardiac abnormalities.
The bottom line is that more the blood sugar and for longer it stays on higher levels, you will have more AGEs and more diabetic complications. AGEs production in diabetic is 60% more than non-diabetic according to the book BloodSugar101 and that makes sense. The less AGEs you produce the better your chances are to avoid diabetic complications and that is a result of near normal sugars around the clock.
This research study from 2012 shows that the chronic complications were least below the a1c of 6%.
https://www.researchgate.net/public...nd_chronic_complications_in_diabetes_mellitus
This is another interesting study of a1c correlation with diabetic complications which shows that an a1c value below 6% is the safe value to target for.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3114320/
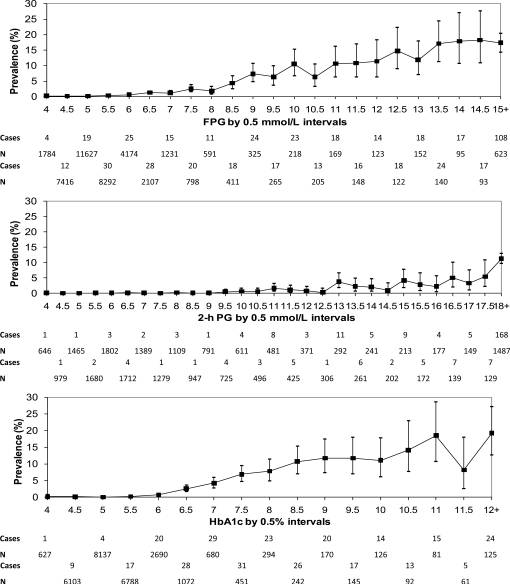
This is perhaps a more interesting study about diabetic retinopathy occurrence at different FPG and A1C levels. Its evident that prevalence of diabetic retinopathy starts when the FPG starts increasing above 5.5 mmol/l level, or when your PPG starts increasing from 9 mmol/l level, or at HBA1C level of 5.5 which seems like a cut point in this study.
Full study is here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3005450/
I could only find the reference to retinopathy complications, but in another study where the researcher correlated neuropathy and CVD as well, the threshold seems to be the same.
My conclusion (and the goals that I would set for myself) after all those months of research is as follows:
- Try to keep your A1C as close to 5% as possible
- Try to keep your fasting BG below 5.5 mmol/l
- Try to keep your post prandial peak below 7 mmol/l
Its important to mention that AGEs are not only produced by glycation but can also be added to your body through dietary sources through what is called Maillard reaction or dAGE, however most of these dietary AGEs are excreted from the body and daily limit of dietary AGEs recommended per day is 15000 units/day (or kU/gm), which sounds very high but just a 90 gm pan fried beef steak contains over 8500 of these units.
A safe and optimal dAGE intake for the purposes of disease prevention has yet to be established. However, in animal studies, a reduction of dAGE by 50% of usual intake is associated with reduced levels of oxidative stress, less deterioration of insulin sensitivity and kidney function with age, and longer life span.
Reducing dAGE may be especially important for people with diabetes, who generate more endogenous AGEs than those without diabetes and for those with renal disease, who have impaired AGE clearance from the body
Its very interesting and a relatively new concept but if you really need to read more details about it, here is a full guide including which food has how many AGEs and what type of cooking methods increase or decrease these AGEs.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3704564/
I would be very interested to hear more about your personal experiences with your glycaemic control, number of years of diabetes and any complications that developed or reversed.
Last edited:

