A quick intro. 65 year old male, type 2 diagnosed Jan 2003. Generally poor control with interludes of low carb, esp 2013 when I effectively put it into remission for about 8 months with very strict low carb. On metformin, dapaglifozin and exenatide. Feb this year suddenly started getting nasty side effects from the metformin and dapaglifozin so stopped them and went strictly low carb, one meal a day. However, BG tested with out of date test strips stubbornly high, 17 to 21 mmol/L. Concerned that endogenous insulin production failing, not sure what was going on as not accurate BG test data. Dropped from a high of about 117kg in 1996 to 78-80kg, 5ft 11, still got some visceral fat to lose but now able to wear the brand new 34" waist cords I bought from C&A a long time ago, loose, need a belt with them. Latest HbA1c was 10.4%.
Met with local practice diabetes nurse and specialist diabetes nurse a week ago and started low dose lantus then; starting with 6 units and steadily increasing dose. I know it's supposed to take 3 days to stabilise but 6 units wasn't having any effect so have slowly titrated dose upwards, now up to 20 units/day. Found various research papers on pubmed advising algorithms for titration of lantus doses, safely following advice found in the scientific literature, recording and analysing results in a spreadsheet. Initially new meter confirmed BGs in upper teens, since starting insulin have been gradually dropping, I hope I can add a graph.
Not sure if I am insulin deficient or still have high insulin resistance, probably both issues but what are the relative contrbutions. The most effective measure so far has been a 44 hour fast from 5pm Mon to 1pm Wed this week (first ever of this length, went better than anticipated!). FBG of 8.2 on 21/4. Back up to 17 this morning after an experiment of about 100g carbs yesterday evening.
I've been searching info on how much lantus a low carbing insulin sensitive T1 requires, ie. if totally dependent upon exogenous basal insulin to cover, say, 20 to 40g daily carbs. How does my usage compare to that and to what extent am I insulin deficient? I'm very familiar with the work of Volek and Phinney and bought both their books years ago; read lots of papers on the whole issue.
I don't want to be using insulin and hope I can wean myself off it after I have got the BG's down. High insulin levels resulting in inflammation resulting in elevated free radical production resulting in decreased levels of highly unsaturated membrane phospholipids which are strongly correlated with insulin sensitivity. So insulin resistance increases resulting in the need for more insulin, seems to be the accepted vicious circle leading to progressive loss of insulin sensitivity. So lower levels of insulin = good, don't really want to be injecting the stuff.
The good news is I've got a new test meter and now have reliable data about BGs.
Working through it and trying to be patient. I'm concerned that my endogenous insulin production is severely reduced and wonder if it can recover given external insulin support. There are several papers in the literature about the long term benefits of intensive early insulin therapy and the restoration of beta cell function when the pancreas is effectively given a holiday. Almost a couple of decades too late for that intervention.
Has anyone else been in the same position, achieved control and been able to progressively wean themselves of insulin therapy? Apologies for the rambling post if youve got this far. I'm sure others must have been in this same position.
You can see from the graph that increasing doses of lantus are giving only a gradual reduction in BGs and it was the 44 hour fast that tanked the numbers down to 8sh. NB strong dawn phenomenon.
Thanks for getting this far.
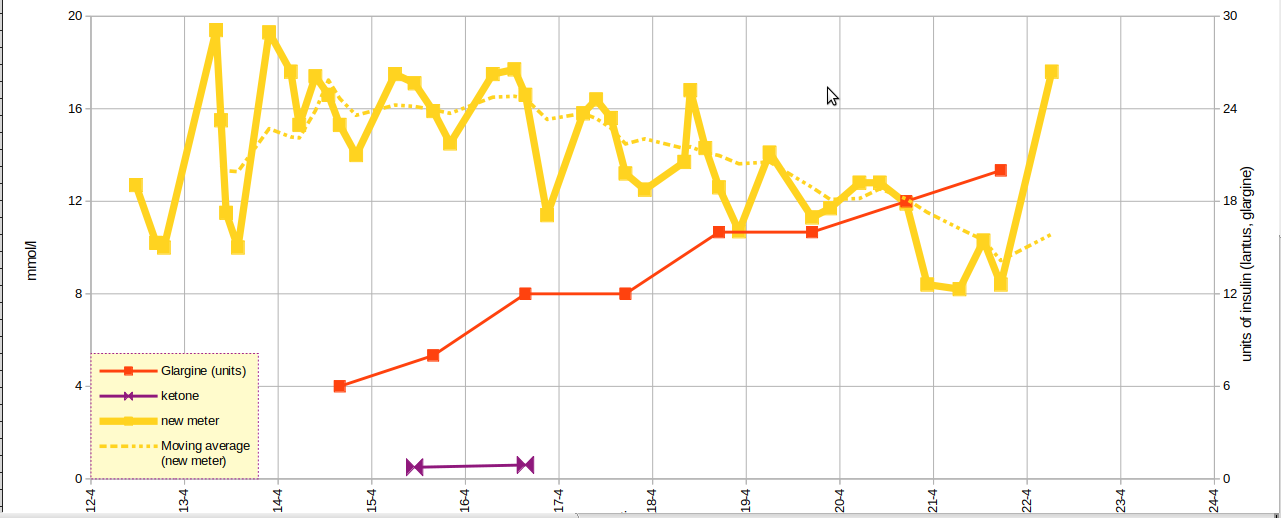
Met with local practice diabetes nurse and specialist diabetes nurse a week ago and started low dose lantus then; starting with 6 units and steadily increasing dose. I know it's supposed to take 3 days to stabilise but 6 units wasn't having any effect so have slowly titrated dose upwards, now up to 20 units/day. Found various research papers on pubmed advising algorithms for titration of lantus doses, safely following advice found in the scientific literature, recording and analysing results in a spreadsheet. Initially new meter confirmed BGs in upper teens, since starting insulin have been gradually dropping, I hope I can add a graph.
Not sure if I am insulin deficient or still have high insulin resistance, probably both issues but what are the relative contrbutions. The most effective measure so far has been a 44 hour fast from 5pm Mon to 1pm Wed this week (first ever of this length, went better than anticipated!). FBG of 8.2 on 21/4. Back up to 17 this morning after an experiment of about 100g carbs yesterday evening.
I've been searching info on how much lantus a low carbing insulin sensitive T1 requires, ie. if totally dependent upon exogenous basal insulin to cover, say, 20 to 40g daily carbs. How does my usage compare to that and to what extent am I insulin deficient? I'm very familiar with the work of Volek and Phinney and bought both their books years ago; read lots of papers on the whole issue.
I don't want to be using insulin and hope I can wean myself off it after I have got the BG's down. High insulin levels resulting in inflammation resulting in elevated free radical production resulting in decreased levels of highly unsaturated membrane phospholipids which are strongly correlated with insulin sensitivity. So insulin resistance increases resulting in the need for more insulin, seems to be the accepted vicious circle leading to progressive loss of insulin sensitivity. So lower levels of insulin = good, don't really want to be injecting the stuff.
The good news is I've got a new test meter and now have reliable data about BGs.
Working through it and trying to be patient. I'm concerned that my endogenous insulin production is severely reduced and wonder if it can recover given external insulin support. There are several papers in the literature about the long term benefits of intensive early insulin therapy and the restoration of beta cell function when the pancreas is effectively given a holiday. Almost a couple of decades too late for that intervention.
Has anyone else been in the same position, achieved control and been able to progressively wean themselves of insulin therapy? Apologies for the rambling post if youve got this far. I'm sure others must have been in this same position.
You can see from the graph that increasing doses of lantus are giving only a gradual reduction in BGs and it was the 44 hour fast that tanked the numbers down to 8sh. NB strong dawn phenomenon.
Thanks for getting this far.


