Your thoughts are bit different from what I normally hear. Hopefully, you can elaborate a bit more to help some of us understand.
You mentioned gluconeogenesis which I understand to be the process of converting energy other than carbs (usually excess protein) into glucose. However, can you touch on how that affects post-exercise "liver dumps?"
It's my understanding that our bodies can only hold about 2000 calories worth of glycogen. That's split up into 500 which is stored in our liver and 1500 spread out through our skeletal muscle. It's my understanding that our livers can decide when to release that 500 (unfortunately, not always when we want it to). However, the 1500 calories in our skeletal muscle cannot be transferred throughout our body. Basically, glycogen in your thighs can replenish lost glycogen in your arms.
It's also my understanding that the 500 calories of glycogen stored in your liver are what cause your blood sugar to spike abnormally. However, those 500 calories can only last so long and probably won't last longer than 1-2 hrs.
Long story short, I think I understand why we have blood sugar spikes within the first hour of exercise, but after a certain point we've depleted our liver glycogen stores which means it couldn't spike our blood sugar until its replenished again.
You're much more qualified to discuss this than I am and I'm hoping you can point out what I'm missing in the equation.
Hi there,
Apologies I haven't replied sooner - I've only just spotted your post.
It sounds as though you already have an excellent understanding of the body's mechanics - that's great that you've taken time to try to understand what goes on in the body with exercise. I'm not sure I'm any more qualified than you to try to make sense of how the body behaves with exercise when you have diabetes, but for the record here are my thoughts:
I tend to keep a mental note of 'carb' storage in the body, vs 'calories' and my figures sound a little different to yours at approx 500g glycogen in the muscles vs 100g in the liver (
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3248697/). Of course this figure is always going to vary - we're all made up differently and have different levels of storage capacity anyway.
It can also be a little misleading to only think in terms of glycogen stored, as the body is also able to run on other sources of energy such as free fatty acids.
So, a potted explanation (trying to keep it simple

)
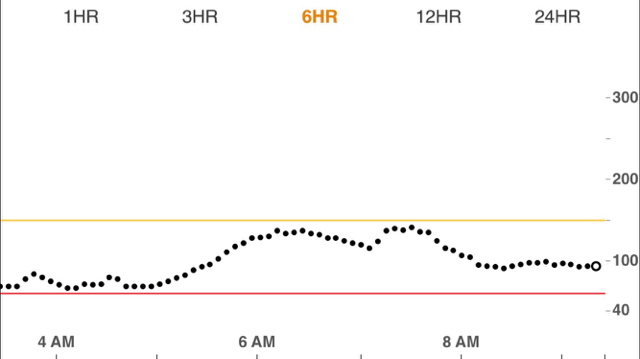
Low/Moderate intensity exercise.
When you begin to exercise, your muscle glycogen become the first port of call. If the exercise is moderate intensity, then these stores will gradually be depleted, and after 15 - 20 mins or so, glucose will begin to be pulled out of the bloodstream. This will result in a gentle fall in blood glucose and this fall will be countered by your liver, which will convert it's easily convertible glycogen stores to glucose (through glycogenolysis) and top your glucose levels up. (Research suggests that the glucose may also come from gluconeogenesis at this point:
http://www.ncbi.nlm.nih.gov/pubmed/15356077) . This is the basic pattern for 'moderate' exercise - where the heart rate hasn't been elevated a great deal. (Remember that glucose isn't the only source of fuel and for low to moderate exercise, fats are a useful source of energy.
A point of interest is also that for anybody without diabetes, the pancreas switches off insulin production when they begin to exercise, as circulating insulin can cause a rapid fall in blood glucose.
Higher intensity exercise
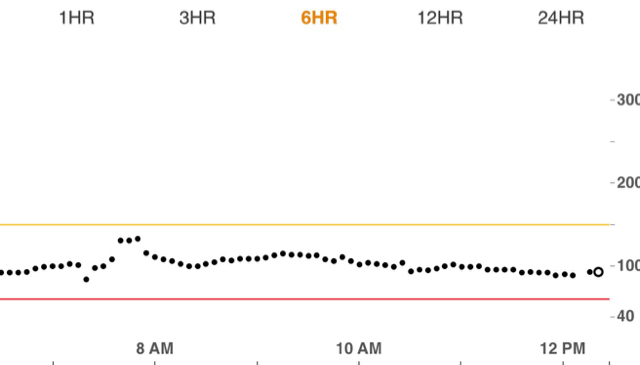
Raise the heart rate, and something quite different happens. Firstly at higher intensities the muscles' favoured fuel source is glucose. With the rise in heart rate comes an automatic stress response within the body which triggers the liver to release glucose into the bloodstream. This source may come from the process of glycogenolysis, gluconeogenesis, or both. Much as you may have '100g' of carb in the form of readily available glycogen for quick release by the liver, gluconeogenesis is the main cause of rising and continuing high levels of glucose in the bloodstream and the liver will continue pumping out glucose for as long as your heart rate is elevated (or until you drop!). So to the point about a liver 'dump' with exercise, it's not so much just a one 'hit'. Whilst the heart rate remains elevated, the liver is still getting the stress signal to release glucose.
A problem of rising bloods comes at the point where you finish your exercise (or you suddenly reduce the muscle work rate), because the liver takes a while to get the message that you've stopped your activity and so continues pumping out glucose. Once finished, you're no longer working your muscles, so the glucose is no longer getting used up and the result is that glucose begins to build up in the bloodstream.
For anybody without diabetes, immediately after exercise (or at any point that there are rising blood glucose levels), their pancreas will release insulin. Insulin not only enhances the rate at which the glucose gets taken up by the muscles, but it can also signal the liver to stop releasing glucose (possibly because glucagon is a hormone involved in the regulation of liver gluconeogenesis, and glucagon and insulin act like a tag team in the pancreas - release one and the other switches off and vice versa).
I don't think it has been studied fully yet, but it seems that for some individuals with diabetes, eating something and taking some insulin after exercise can mimic this action (and so help switch off gluconeogenesis) after exercise.

Phew - sorry if that was a bit tedious! The point is that although there is a liver 'dump' to a stress response caused by an elevated heart rate, the liver will actually keep pumping out glucose indefinitely over and above any easily accessible glycogen stores and if I remember correctly, it is generally understood that elevated glucose levels in T1D are always attributed to gluconeogenesis.
Hope that helps a bit.