It happens exactly to me. My weight rapidly increases if I have carbs.Well as I said above I fitted all their criteria for remission in terms of weight loss and as soon as I increased carbs more than the very rare occasion it all started to go backwards again. Good luck if you achieve it but seeing as the original Newcastle trials were only about 50% successful I’m not sure I believe the reported conversation claiming 100% success.
-
Guest - w'd love to know what you think about the forum! Take the 2025 Survey »
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Carbs-independent remission
- Thread starter chrisjohnh
- Start Date
What I was told during discussion with the principal investigator is that after the crash-diet phase the remitters resumed eating that was reduced somewhat (so not literally free) but with unrestricted and freely chosen macronutrient composition, and that the remitters maintained their position for the rest of the two-year period - and that not a single one of them went on low carbs. Well, I don’t know what to make of it all, but I’m minded to up my carbs from 125 to 180 for 3 months and see what happens. I suspect my A1c will rise but who knows? Just curious to see if remission life is possible without constant fear of catching sight of a bread crumb or half a bana
I really think they need to do further research to be honest. Once a diabetic, always a diabetic and in remission through low carbing. It cannot be cured, we have a metabolic disorder which is maintained through diet, also for me. I need to stay very active, as I only need to look at a carb and I put weight on.I can tell you that their unswerving belief is that if T2Ds clear out all their ectopic fat soon after diagnosis then most of them will get their A1c below 48 (I know, not the biggest deal) and can keep it there indefinitely by carefully not regaining weight whilst otherwise eating what they like. They would argue that with a well-resurrected pancreas one should not produce excess insulin in response to a high dollop of carbs and therefore should not suffer an adverse effect such as weight regain. I think their view is that if you’ve still not cleared your ectopic fat then keeping your A1c low merely by low carbing is just a “poor man’s kind of remission”, just a trivial demo of the obvious that you won’t get high flames from the fire in your innards simply by desisting from throwing fuel on it, even though it’s still smouldering underneath and will eventually create a crisis. Now I don’t know what the reality is here because the research is still too sparse and low scale. But I may do my own n=1 non-RCT experiment before long.
ajbod
Well-Known Member
I have noticed with myself, and i also think that if we low carb properly for a while, ours Pancreas will recover slightly from the thrashing it has had, from our hyperinsulemia due to Insulin resistance, and our resistance will improve. i find that i can have a carby meal and have a proper insulin response without raised sugars. BUT i also know that this will rapidly go to £$%^, if i continued eating that way.
I have lost 30kg since diagnosis 10 years ago. If I have carbs my HbA1c goes up and I am no longer in remission. It's 52 now.
Edit: I have lost 6 kgs since my last HbA1c so it isn't weight gain that's taken me out of remission, it's the carbs.
Edit: I have lost 6 kgs since my last HbA1c so it isn't weight gain that's taken me out of remission, it's the carbs.
Last edited:
If that's the case, that it has not been fully published, then it can be kicked right out of the ball park. No one can make an assessment without all the facts. I have a feeling that it is a failure and those who went into remission have now not in control. Its doomed to fail in the first place.I would add that it’s a pity that the complete picture of what the DiRECT remitters were eating during their second year has not been fully published, and may not have been even fully ascertained. This gap so far makes it hard for the rest of us to make an incisive assessment of the trial and of its implications for our own future T2D management. But I may do my own little experiment as I mooted earlier in the thread.
Why do you think that, We all think the same. first thing, is to reduce glucose levels and to do this was to reduce the carbs, by reducing the carbs Glucose levels are reduced and weight loss follows. This has happened to most of us,, therefore a large example of this. Dr Unwin has a lot of success with his diabetic patients. You could always write to him for his input over the matterMmmm … sample size a little on the low side perhaps !
Well let us know how you do. Include the complete break down of what you did and the foods you ate. That would be intesting.The latter para misinterprets my intent, which is to see whether raising carbs will raise my A1c. My weight will remain constant because I will make it so by other adjustments.
Any Ideas what the statistics are now. It is only 2 years, which is not a long time at all. I am 9 years in, which to me is a very long time to stay in remission. I would not follow their recommendations at all. I do not follow the recommendation of needing to eat carbs with every meal by the diabetic nurses.Is this a fair summary of DiRECT? My understanding is that most of those who were in remission at 1 year had remained so at 2 years. This is not “temporary” remission for the majority - so far, anyway.
Oldvatr
Expert
- Messages
- 8,453
- Type of diabetes
- Type 2
- Treatment type
- Tablets (oral)
If we put aside the ultra low calorie diets (eg Newcastle) and examine the track record for bariatric surgery, which was what prompted Roy Taylor to so the trials in the first place, then we see temporary remission , but then a creep back to diabetic levels within a fairly short time after the procedure. Gastric banding is next to useless for diabetes, and is a weight loss program therapy. The Roux-Y procedure is slightly more successful for diabetics, but is still low success rate and not permanent either. Some GB can be reversed, but generally once it is modified then you are stuck with it, i.e. it should be permanent but it isn't.
Now look at the ND diet - it emulates what the GB does in terms of calorie intake and gives some respite from diabetes, but it too is not showing long term unfettered success. The therapy needs to be followed by strict low calorie diet to maintain weight loss, and this follow on diet is what determines the ultiate long term success or not,. So the advice is to have very reduced portion size again to menulate the GB procedure. So like the GB procedure, we might reasonably expect similar results i.e. an upward trend in both weight and glucose levels. The difference s that with diet, it is possible to easily revert to old life habits and does not require surgical interventipn to reverse the diet.
Now look at the ND diet - it emulates what the GB does in terms of calorie intake and gives some respite from diabetes, but it too is not showing long term unfettered success. The therapy needs to be followed by strict low calorie diet to maintain weight loss, and this follow on diet is what determines the ultiate long term success or not,. So the advice is to have very reduced portion size again to menulate the GB procedure. So like the GB procedure, we might reasonably expect similar results i.e. an upward trend in both weight and glucose levels. The difference s that with diet, it is possible to easily revert to old life habits and does not require surgical interventipn to reverse the diet.
What also needs acknowledging is that the ND diet used in the study is actually Low Carb and only just above keto for most people. Does not matter which shakes are used, Optifast. Exante, or Cambridge they are low carb.And I too have “low carbed” (125-130g) for (two) years, with A1c stable so far. But with those who have had to keep stepping their carbs ever further down I would be curious to know whether they had not originally cleared their pancreatic fat to the maximum possible and thus had only been living on borrowed time. What does need acknowledging by the low carb believers is that the DiRECT two-year remitters maintained their remission without low carbing at all. This cannot be dodged.
Oldvatr
Expert
- Messages
- 8,453
- Type of diabetes
- Type 2
- Treatment type
- Tablets (oral)
I am simply peer reviewing. Where does Taylor identify a peer review took place? Who reviewed his work? I repeat, the style of reporting his results falls short of what I would expect from an academic institution. As a scientist, you should also feel uncomfortable about this.Of course all scientists get some things wrong and we depend upon experimentation, critique and peer review to tease out the flaws and to make progress. I think you verge on being unkind to Taylor by giving the impression that he commits wilful obscuration or avoidance of inconvenient considerations, or that his many collaborators do also. That doesn’t ring true with me. But your penultimate para hits all the right nails on the head, this has been my exact frustration with that research programme and its reporting to date.
Oldvatr
Expert
- Messages
- 8,453
- Type of diabetes
- Type 2
- Treatment type
- Tablets (oral)
I thinl this is relevant, from the DIRECT 2 year follow up
"In a post-hoc analysis of the whole study population, of those participants who maintained at least 10 kg weight loss (45 of 272 with data), 29 (64%) achieved remission; 36 (24%) of 149 participants in the intervention group maintained at least 10 kg weight loss."
The 64% remission group is of the 45 that maintained weight loss, out of the 272 that took part in the DIRECT study.
"In a post-hoc analysis of the whole study population, of those participants who maintained at least 10 kg weight loss (45 of 272 with data), 29 (64%) achieved remission; 36 (24%) of 149 participants in the intervention group maintained at least 10 kg weight loss."
The 64% remission group is of the 45 that maintained weight loss, out of the 272 that took part in the DIRECT study.
chrisjohnh
Well-Known Member
- Messages
- 286
- Type of diabetes
- Type 2
- Treatment type
- Diet only
The fundamental observation of the DiRECT investigators is that clearing out the ectopic fat results in hepatic and pancreatic functional normalisation, including first phase response. That is, other than an underlying genetic susceptibility to regaining ectopic fat upon weight regain, one’s position should be as for a non-diabetic, i.e. not having to treat carbs per se as some kind of poison. Well, as I said, I am not certain about all that, but I shall do my 3-month elevated carb experiment to get at least an answer for myself and I will certainly present the outcome and a comprehensive account of the regimen adopted. My hunch is that raising my carbs from 130g to 180g will yield no significant difference, but we will see!I thinl this is relevant, from the DIRECT 2 year follow up
"In a post-hoc analysis of the whole study population, of those participants who maintained at least 10 kg weight loss (45 of 272 with data), 29 (64%) achieved remission; 36 (24%) of 149 participants in the intervention group maintained at least 10 kg weight loss."
The 64% remission group is of the 45 that maintained weight loss, out of the 272 that took part in the DIRECT study.
chrisjohnh
Well-Known Member
- Messages
- 286
- Type of diabetes
- Type 2
- Treatment type
- Diet only
To be clear here, if you increase your carb intake then do you also reduce your fat and/or protein intake? I mean by amount in g, not by percentage composition?It happens exactly to me. My weight rapidly increases if I have carbs.
chrisjohnh
Well-Known Member
- Messages
- 286
- Type of diabetes
- Type 2
- Treatment type
- Diet only
Well it is standard practice that the reviewers of journal submissions are not identified to the authors, so we cannot know who reviewed the many papers published by that team.I am simply peer reviewing. Where does Taylor identify a peer review took place? Who reviewed his work? I repeat, the style of reporting his results falls short of what I would expect from an academic institution. As a scientist, you should also feel uncomfortable about this.
Oldvatr
Expert
- Messages
- 8,453
- Type of diabetes
- Type 2
- Treatment type
- Tablets (oral)
You are comparing apples with bananas. as I understand it you are currently low carbing, so your start point for comparison is not the same as most of the ND participants. By all means, experiment. i hardly think 180g carbs is a reflection of unlimited carbs as stated in your OP. It is certainly not gay abandon levels. You will probably see a rise in average bgl levels, so please make sure you track the average daily level. As it happens, I in my n=1 journey eat around 200 g per day with a medium high fat content, and my weight has been pretty static for several years now at 64kg.The fundamental observation of the DiRECT investigators is that clearing out the ectopic fat results in hepatic and pancreatic functional normalisation, including first phase response. That is, other than an underlying genetic susceptibility to regaining ectopic fat upon weight regain, one’s position should be as for a non-diabetic, i.e. not having to treat carbs per se as some kind of poison. Well, as I said, I am not certain about all that, but I shall do my 3-month elevated carb experiment to get at least an answer for myself and I will certainly present the outcome and a comprehensive account of the regimen adopted. My hunch is that raising my carbs from 130g to 180g will yield no significant difference, but we will see!
You did not get my point in my last post. The number of people that were in remission at 2 years is only 6.8% of the number that started, and about half of those in remission seem to be control cohort members using medication, not ND dieters off medication.
chrisjohnh
Well-Known Member
- Messages
- 286
- Type of diabetes
- Type 2
- Treatment type
- Diet only
I agree that my start point is not comparable to the ND position, but it is not my intent to construct any such comparison. I have just the narrow aim of testing whether, from where I stand now, I can up my carbs without detriment. I do already know from previous experimentation that my 3 months on 100g (ending with A1c=42) followed by 3 months on 135g left my A1c virtually unaltered (ending with A1c=40). And I agree that going up to 180g will hardly be radical - but it might allow me some welcome extra latitude. Your 200g is a very good level. I too weigh 64kg.You are comparing apples with bananas. as I understand it you are currently low carbing, so your start point for comparison is not the same as most of the ND participants. By all means, experiment. i hardly think 180g carbs is a reflection of unlimited carbs as stated in your OP. It is certainly not gay abandon levels. You will probably see a rise in average bgl levels, so please make sure you track the average daily level. As it happens, I in my n=1 journey eat around 200 g per day with a medium high fat content, and my weight has been pretty static for several years now at 64kg.
You did not get my point in my last post. The number of people that were in remission at 2 years is only 6.8% of the number that started, and about half of those in remission seem to be control cohort members using medication, not ND dieters off medication.
The matter of the 2-year DiRECT remitters: I may be in error, but my reading of the published data (e.g. in the 2019 paper in Lancet Diabetes and Endocrinology, 7(5), pp. 344-355, and also in other papers) is that at 24 months 53 (36%) of the intervention participants (total 149 at baseline) had remission of diabetes, being a subset of those 68 who had been in remission at 12 months. So I don't see where your 6.8% comes from. I also am not clear about the medication factor within the intervention cohort - there are some ambiguities among the various papers.
I sense that the DiRECT investigators take the view that those T2Ds who are very carb-intolerant, and so really do need to keep their carbs well down, are in that position for any of several reasons, including (a) they never did clear their ectopic fat, or (b) they did, but did so too long after diagnosis, or (c) they have some other or additional metabolic deficiency, or (d) are just inexplicably unlucky. And equally I sense that their view is that those who achieve "real" remission, having become normoglycaemic purely through clearing ectopic fat, have no need whatever to even think about carbs subsequently, never mind reduce them. But whether they are right, I cannot tell.
Last edited:
Ronancastled
Well-Known Member
- Messages
- 1,234
- Type of diabetes
- Type 2
- Treatment type
- Diet only
@Oldvatr I'm a Taylor advocate but like you I can pick holes in his work.
Before ReTune, before Direct, we had Counterpoint, published back in 2012.
https://eprints.ncl.ac.uk/file_store/production/175328/FA1F5CAA-078D-4CDB-8DC3-49CE08B40C72.pdf
This was the one & only time he ever submitted his successful candidates to a 75g OGTT post remission.

I don't know how you could judge these candidates as being in remission, 10.3 @ 2 hours on the gold standard 75g OGTT is very very prediabetic.
No record of where they were @ 1 hour either, perhaps there was no lab draw, perhaps he didn't see fit to publish.
Either way he never repeated this test on any of his follow up studies.
Before ReTune, before Direct, we had Counterpoint, published back in 2012.
https://eprints.ncl.ac.uk/file_store/production/175328/FA1F5CAA-078D-4CDB-8DC3-49CE08B40C72.pdf
This was the one & only time he ever submitted his successful candidates to a 75g OGTT post remission.

I don't know how you could judge these candidates as being in remission, 10.3 @ 2 hours on the gold standard 75g OGTT is very very prediabetic.
No record of where they were @ 1 hour either, perhaps there was no lab draw, perhaps he didn't see fit to publish.
Either way he never repeated this test on any of his follow up studies.
chrisjohnh
Well-Known Member
- Messages
- 286
- Type of diabetes
- Type 2
- Treatment type
- Diet only
Indeed so. Given the growing aspiration that GPs should shift much more emphasis towards attempting remission, and given how important it would become to maintaining that, there will need to be much more incisive research done - and widely and reproducibly - on the basis, tactics and assessment of remission, together with write-ups that provide clear data for HCPs and patients alike. I think all of us here who have been discussing this thread are in agreement that we need much better analysis than what can be gleaned from the two dozen or so papers emerging so far from DiRECT. But science is under funding stress, university life is much harder in very many ways than 40 years ago, so we are fortunate that people like Taylor and their impoverished PhD students and postdoc researchers are in the game at all, and we should all be sensitive to that, I suggest. Meanwhile we all plod on with our self-experimentation.@Oldvatr I'm a Taylor advocate but like you I can pick holes in his work.
Before ReTune, before Direct, we had Counterpoint, published back in 2012.
https://eprints.ncl.ac.uk/file_store/production/175328/FA1F5CAA-078D-4CDB-8DC3-49CE08B40C72.pdf
This was the one & only time he ever submitted his successful candidates to a 75g OGTT post remission.
View attachment 57687
I don't know how you could judge these candidates as being in remission, 10.3 @ 2 hours on the gold standard 75g OGTT is very very prediabetic.
No record of where they were @ 1 hour either, perhaps there was no lab draw, perhaps he didn't see fit to publish.
Either way he never repeated this test on any of his follow up studies.
Oldvatr
Expert
- Messages
- 8,453
- Type of diabetes
- Type 2
- Treatment type
- Tablets (oral)
Indeed. It is interesting to note the weight gain in just 12 weeks. As regards remission, Taylor has his own definitopn of remissio that differs from the rest of the world. He ignores prediabetes as being a classification. Also, there was no check on medication use post intervention, and at least some 40% continued to use their diabetic meds. The rest of the world requires remission to be sans medication. and a yearly HbA1c to also be non diabetic.@Oldvatr I'm a Taylor advocate but like you I can pick holes in his work.
Before ReTune, before Direct, we had Counterpoint, published back in 2012.
https://eprints.ncl.ac.uk/file_store/production/175328/FA1F5CAA-078D-4CDB-8DC3-49CE08B40C72.pdf
This was the one & only time he ever submitted his successful candidates to a 75g OGTT post remission.
View attachment 57687
I don't know how you could judge these candidates as being in remission, 10.3 @ 2 hours on the gold standard 75g OGTT is very very prediabetic.
No record of where they were @ 1 hour either, perhaps there was no lab draw, perhaps he didn't see fit to publish.
Either way he never repeated this test on any of his follow up studies.
There is a seperate study he did using IVGTT techniques and an argenine block to measure insulin response. The problem with that study was that he combined two different tests into one continuous session, without a break and this in my opinion skewed the results since it is clear from the graphs that the second test started before the first test had washed out. Also the graphs he published seem to show a Stage #1 insulin response, but the timings on the graph are way out, Phase#1 is triggered by amylase release into the saliva starting to break down the simple starches and sugars before reaching the stomach, so there is a rush of glucose immediately available. This enters the blood stream some 6 minutes after eating starts. It lasts less than 15 minutes. But his first IVGTT measurement seems to be taken at 30 mins which is way past the peak. He is also using IVGTT, so is missing the amylase trigger and any other enzyme activity that may be associated with oral admiistration such as GLUT=4 The other problem seems to be that he uses insulin rate as the measurement parameter when really it should be the area under the curve. I have already commented on his use of a special way of reporting the results where he divides the normal insulin rate by effectively BMI so making it weigh dependant. So it is valid when comparing member within the group, but totally skewed by a weight loss intervention over time. Of course a 15kg weight loss showed improved response - its in the maths.
Ronancastled
Well-Known Member
- Messages
- 1,234
- Type of diabetes
- Type 2
- Treatment type
- Diet only
@Oldvatr Agreed on the above.
I've noticed too that the non-diabetic comparator group had an average A1c of 5.7%(38)
That's pre-diabetic in American money so you'd have to assume some level of insulin resistance there too.
I believe he was matching them for age & weight so I suppose that's where the Eatwell Plate gets you.
I recall the Dutch survey of the average adult population revealed similar results.
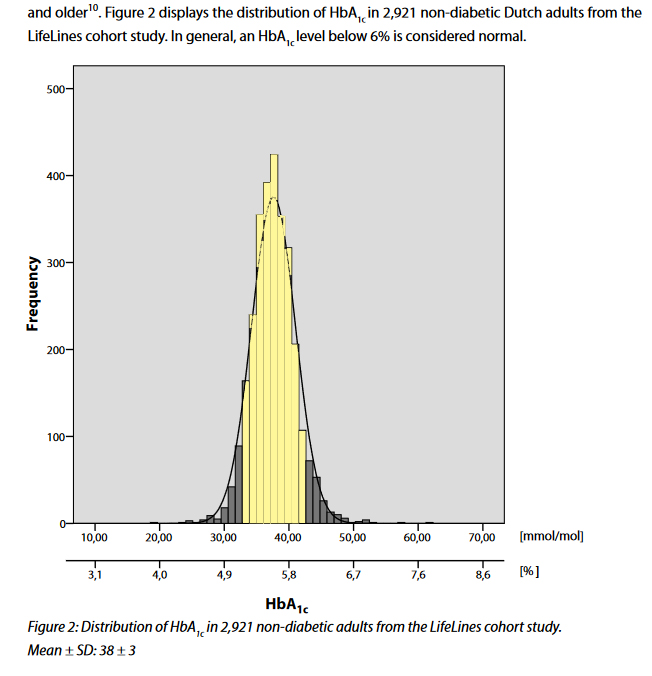
No wonder a 3rd of Americans are pre-diabetic when the average A1c of adults falls on the diagnostic cutoff line.
Further to this, it's no wonder doctors just ignore it as an issue.
I've noticed too that the non-diabetic comparator group had an average A1c of 5.7%(38)
That's pre-diabetic in American money so you'd have to assume some level of insulin resistance there too.
I believe he was matching them for age & weight so I suppose that's where the Eatwell Plate gets you.
I recall the Dutch survey of the average adult population revealed similar results.
No wonder a 3rd of Americans are pre-diabetic when the average A1c of adults falls on the diagnostic cutoff line.
Further to this, it's no wonder doctors just ignore it as an issue.
