I‘m right there with you @Antje77 with that one. I’m minded to think I have a problem with enzymes or something. It’s definitely fats that are the issue for me, so I’m guessing it could be affecting other chemicals too. I’ll be seeing my Dr in the New Year I will know more then.I'm not sure if I asked this before, but with your unclear type of diabetes which may or may not be T3C, and your intolerance to fats, have you ever had tests for EPI? It may be you need creon with your food to properly digest.
-
Guest - w'd love to know what you think about the forum! Take the 2025 Survey »
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Is it possible to have LADA/1.5 with high C peptide?
- Thread starter Vectian
- Start Date
Despite my consultant not being able to answer the question about how is it possible to have LADA (i.e. insufficient insulin is causing the high BS) but normal C peptide and giving me fudge answers, I think I may have worked it out:Extremely interesting to read and thank you for sharing.Been also very enlightening reading others posts and am grateful for this platform. I seem to be somewhat an Enigma myself with the Endocrinologist and have him scratching his head due to a normal C Peptide but glucose kept spiking and waking in the morning to high glucose levels often 11.
I have been diagnosed with LADA Type 1.5 earlier this year and have the anti bodies which confirm this. But recently things have gotten worse so just started slow acting insulin. HBA1c jumped up and glucose spiking and was tired. But the good,old C Peptide was normal (did a non fasting test).
Going to try and get back to better management of my diet especially my evening meal. I had been following a more Keto type diet but this year slipped into eating a few more carbs, but not much. I am slim build.
I went straight to slow acting insulin and this has indeed stopped the morning waking spike.
Anyway, I love all the theories and am glad I am not the only one who seems to leave the Endos scratching their heads.
Personally, I really don’t want to take fast acting insulin at the moment as well as the slow as my concern is hypos. Endo not pushing it either and being very supportive.
My theory being if I have a good day and kick out more insulin from my own pancreas and take fast acting insulin as well as my slow acting, I will no doubt have a hypo. It’s a bit of trial and error at the moment for me and I feel like I am just lucky I can be experimental as clearly still have some insulin production.
I also figure steering clear of glucose spiking foods and eating things with fibre and healthy fat, should help matters especially with my evening meal ( potatoes, even sweet potatoes seem to be an issue for me).
Shame I can’t have a permanent glucose monitor yet from the NHS so I just keep pricking my finger and making observations.
I wish there was more information out there, but I did hear from the Endo that LADA is on the increase and it makes you wonder why? Better testing maybe or perhaps another reason?
There are 2 ways to do a C peptide test - fasting and stimulated (after eating). When your C peptide test is done, it is usually fasting. At diagnosis that will likely be with very high BS. A non diabetic would have a fasting BS of say around 5, as you haven't eaten the insulin demand is at it's lowest. The amount of C peptide produced would normally fall within the ranges they give you.
BUT if you do the test and your BS is much higher (mine was around 12) that is higher than a non diabetic would ever go even after eating a heavy carb meal, so your pancreas is constantly trying to release insulin and bring that down, so it's at maximum insulin demand not minimum. So therefore the result should be compared to normal ranges of stimulated C peptide, not fasting. Like a non diabetic who has just eaten a really sugary or carb heavy meal. The stimulated range can go much higher, my consultant said to 6000 or beyond. So my result of 1080 is completely normal when compared to fasting C peptide ranges, but on the low side when compared to stimulated ranges. Hope that makes sense!
With the insulin, my experience is the long lasting insulin kept giving me hypos overnight, not the bolus. It never happened that I dosed for the meal and my own insulin overshot it and hypo, I don't think it works like that. If insulin is detected the pancreas doesn't ignore that and try and produce the equivalent amount itself. As long as you dose correctly, it stays in range fairly easily. I had insulin for 4 weeks, only 1 week of long acting because it made me feel terrible, then 3 weeks of just bolus which was better. And 8 months since with no insulin or anything, although it may be time to add a little back in. The vast majority of LADAs are on some insulin in the honeymoon, it's only when you have very little production that it's over and you are 100% insulin dependant.
See my last reply to LADA enigma, I think that explains how this can be (the same situation with me) and perhaps solves the enigma!Because it really does not make sense @rayq81. I’m trying to get my head around what is going on with a pancreas that is clearly producing insulin, but not enough to suppress your blood sugars. Is it a damaged pancreas, but what’s with the GAD antibodies? That’s why I wondered about the Thyroid. An autoimmune attack on your Thyroid would also produce GAD antibodies - GAD65. It’s a marker for , as we know, t1 but also Graves’ disease, Hashimoto thyroiditis, pernicious anemia, epilepsy and Addison’s disease. I’m not for a moment suggesting these are in play, but that GAD antibodies are produced from a T cell attack on other areas of the body too.
I’m sure you have looked into all this. My understanding, and please anyone correct me if I’m wrong, but an attack on the pancreatic islet cells would kill them off. So there would be a deficit in C-Peptides. In other words your beta cell mass would be severely compromised, and with the loss of these insulin producing islet cells they would be unable to replenish. Are you in a honeymoon phase, alongside insulin resistance? Maybe the medical establishment does not yet understand fully the mechanisms by which late onset T1 progresses. So just a few thought on this.
I’ve incorporated the second link as it lists other autoimmune disorders that produce the GAD65 marker.
https://www.sciencedirect.com/science/article/abs/pii/B9780444563781000460
https://www.mayocliniclabs.com/api/sitecore/TestCatalog/DownloadTestCatalog?testId=81596
Chris24Main
Well-Known Member
- Messages
- 1,024
- Type of diabetes
- I reversed my Type 2
- Treatment type
- Diet only
Not sure I buy that - I've been very low insulin for the entire year, meaning that the way I've been eating is entirely about not stimulating insulin - on my recent test of this with a CGM, every single raise in blood glucose was as a result of doing something, never on account of eating something. Thus, my C-Peptide should be very small right now, whether I've eaten or not.Despite my consultant not being able to answer the question about how is it possible to have LADA (i.e. insufficient insulin is causing the high BS) but normal C peptide and giving me fudge answers, I think I may have worked it out:
There are 2 ways to do a C peptide test - fasting and stimulated (after eating). When your C peptide test is done, it is usually fasting. At diagnosis that will likely be with very high BS. A non diabetic would have a fasting BS of say around 5, as you haven't eaten the insulin demand is at it's lowest. The amount of C peptide produced would normally fall within the ranges they give you.
BUT if you do the test and your BS is much higher (mine was around 12) that is higher than a non diabetic would ever go even after eating a heavy carb meal, so your pancreas is constantly trying to release insulin and bring that down, so it's at maximum insulin demand not minimum. So therefore the result should be compared to normal ranges of stimulated C peptide, not fasting. Like a non diabetic who has just eaten a really sugary or carb heavy meal. The stimulated range can go much higher, my consultant said to 6000 or beyond. So my result of 1080 is completely normal when compared to fasting C peptide ranges, but on the low side when compared to stimulated ranges. Hope that makes sense!
With the insulin, my experience is the long lasting insulin kept giving me hypos overnight, not the bolus. It never happened that I dosed for the meal and my own insulin overshot it and hypo, I don't think it works like that. If insulin is detected the pancreas doesn't ignore that and try and produce the equivalent amount itself. As long as you dose correctly, it stays in range fairly easily. I had insulin for 4 weeks, only 1 week of long acting because it made me feel terrible, then 3 weeks of just bolus which was better. And 8 months since with no insulin or anything, although it may be time to add a little back in. The vast majority of LADAs are on some insulin in the honeymoon, it's only when you have very little production that it's over and you are 100% insulin dependant.
However - this time last year - my "normal" levels of both blood glucose and circulating insulin were much, much higher, so even in a fasted state (at least my understanding of what a fasted state was last year - really meaning "in the morning after a normal sleep") my insulin levels would have been sky high compared to now.
Fundamentally, C-Peptide is just a measure of whether the pancreas is capable of producing insulin - the C-Peptide itself is just a byproduct. Think of a rugby post. The construction of insulin is like the two posts and the cross-bar. Once they are assembled, the body discards the cross-bar, and the two posts go off to do all the things insulin does. That discarded cross-bar is C-Peptide. So - the test shows up any insulin made, not injected. The timing then is more about how long your body takes to clear up the discarded bits than it is about the rate of production of insulin - though clearly it should be highest shortly post a heavy carb meal - regardless of your insulin sensitivity.
I was explicitly asked to have a heavy-carb meal, then take urine about 2 hours after, and this was the basis of my C-Peptide. I was also injecting, and the purpose of the test was to see whether I was really T2 (which you will know I was from the other thread).
It's kind of the same discussion - and I had some pretty edgy conversations with my specialist consultant, I can tell you.... though I do feel conflicted about it, we disagreed on a lot, but I very definitely credit her with saving my life... anyway, my thought was - look, this test shows that my pancreas is still working... indeed, some of the responses I was seeing on my CGM just could not make sense if there wasn't some endogenous insulin... so that being the case, I know that I can safely reduce my insulin level (ie, being free of the concern of ketoacidosis, which seemed to be the major concern among my support team, but I knew that I hadn't seen any sight of a ketone at that point) -
Therefore, for me - it stopped being a question of "how can it be a form of T1 with high C-Peptide" - it was just insulin resistance, like everyone else.
I'm personally suspicious about the "honeymoon" thing, because I was on that track - once you start with insulin, you can (I did) find that the dosage started to go up - which would be consistent with a honeymoon period coming to an end - but it was just that I was taking in too much, which was increasing the circulating insulin, thus exacerbating the insulin resistance...
The support team are only (in my experience) focused on whether your blood glucose is in range - and it probably will be with sufficient insulin - but you will not be doing yourself any favours by having high circulating insulin. The medical doctrine is to control glucose, but as a person, if you can do it safely - there are significant benefits to bringing the insulin level down.
As I understand it, you are an example of someone who was diagnosed T1 but are actually T2, this is pretty rare and usually happens the other way around. So if you are T2 yes injecting insulin is definitely the wrong thing, the issue is too much insulin and therefore insulin resistance. But a T2 C peptide would be high or high normal, the issue is not insufficient production but insulin resistance. This is why when I was initially put on insulin wating the ridiculous 6 weeks for antibody tests, I didn't want to be on insulin as if I was T2 that would make it worse. "it was just insulin resistance, like everyone else" - everyone else with T2, we are are talking about the mechanism of T1 here. Incidentally, if you have cholesterol results you can work out your insulin resistance with reasonable accuracy with fasting BS and triglyceride number, look up triglyceride index calculators.Not sure I buy that - I've been very low insulin for the entire year, meaning that the way I've been eating is entirely about not stimulating insulin - on my recent test of this with a CGM, every single raise in blood glucose was as a result of doing something, never on account of eating something. Thus, my C-Peptide should be very small right now, whether I've eaten or not.
However - this time last year - my "normal" levels of both blood glucose and circulating insulin were much, much higher, so even in a fasted state (at least my understanding of what a fasted state was last year - really meaning "in the morning after a normal sleep") my insulin levels would have been sky high compared to now.
Fundamentally, C-Peptide is just a measure of whether the pancreas is capable of producing insulin - the C-Peptide itself is just a byproduct. Think of a rugby post. The construction of insulin is like the two posts and the cross-bar. Once they are assembled, the body discards the cross-bar, and the two posts go off to do all the things insulin does. That discarded cross-bar is C-Peptide. So - the test shows up any insulin made, not injected. The timing then is more about how long your body takes to clear up the discarded bits than it is about the rate of production of insulin - though clearly it should be highest shortly post a heavy carb meal - regardless of your insulin sensitivity.
I was explicitly asked to have a heavy-carb meal, then take urine about 2 hours after, and this was the basis of my C-Peptide. I was also injecting, and the purpose of the test was to see whether I was really T2 (which you will know I was from the other thread).
It's kind of the same discussion - and I had some pretty edgy conversations with my specialist consultant, I can tell you.... though I do feel conflicted about it, we disagreed on a lot, but I very definitely credit her with saving my life... anyway, my thought was - look, this test shows that my pancreas is still working... indeed, some of the responses I was seeing on my CGM just could not make sense if there wasn't some endogenous insulin... so that being the case, I know that I can safely reduce my insulin level (ie, being free of the concern of ketoacidosis, which seemed to be the major concern among my support team, but I knew that I hadn't seen any sight of a ketone at that point) -
Therefore, for me - it stopped being a question of "how can it be a form of T1 with high C-Peptide" - it was just insulin resistance, like everyone else.
I'm personally suspicious about the "honeymoon" thing, because I was on that track - once you start with insulin, you can (I did) find that the dosage started to go up - which would be consistent with a honeymoon period coming to an end - but it was just that I was taking in too much, which was increasing the circulating insulin, thus exacerbating the insulin resistance...
The support team are only (in my experience) focused on whether your blood glucose is in range - and it probably will be with sufficient insulin - but you will not be doing yourself any favours by having high circulating insulin. The medical doctrine is to control glucose, but as a person, if you can do it safely - there are significant benefits to bringing the insulin level down.
However with the explanation for how you can have normal C peptide but be LADA I wasn't talking about your situation as you aren't LADA. I was talking about the other person (and me) as a way of explaining that seemingly conflicting result, which I struggled to understand ages.
Chris24Main
Well-Known Member
- Messages
- 1,024
- Type of diabetes
- I reversed my Type 2
- Treatment type
- Diet only
Again - I was diagnosed and treated as a late onset type 1 for a year -
I was LADA - and I could easily have had this same conversation the other way around. It's only in hindsight that I can say that I was actually T2. Indeed this is rare, but my point is - the response of the medical world was to give me the treatment appropriate for a T1 - insulin - and had it not been for one consultant who forced the issue with a C-Peptide... I would still be on insulin, and I would still firmly believe that I was a type 1 with a failed pancreas - all the data to hand would back it up - but it would be wrong.
and - understand - at that moment, I was a late onset Type 1 with a positive C-Peptide - I was in precisely the same position as you both.
I cannot - and am not - trying to diagnose you; but I cannot help but wonder how often what happened to me, is actually the case for others who did not benefit from a bolshy consultant who was not prepared to sit back and scratch her head, but instead re-diagnosed me. As you say - it's rare. I was even warned that it was rare and considered dangerous to re-diagnose a T1 as T2 for at least a year, simply due to the dangers of removing insulin unless you are 100% sure there is still an internal supply.
I'm not even saying that you are wrong - hell, you know your own body better than I can. But - you either have a complicated situation that baffles medical understanding ... or the initial diagnosis may be wrong and the answer is simple, as it was for me.
For me - normal C-Peptide = functioning pancreas = cannot be T1 - so go full effort into trying for remission, what do you have to lose. (provided you can do it safely, and I was convinced I could based on what I could see from my CGM).
Please understand - I'm in no way trying to be critical. It's really that for me - the entirety of the medical profession had me pegged for a lifetime of insulin - except one person. And I feel so lucky to have bumped into that one person.
I was LADA - and I could easily have had this same conversation the other way around. It's only in hindsight that I can say that I was actually T2. Indeed this is rare, but my point is - the response of the medical world was to give me the treatment appropriate for a T1 - insulin - and had it not been for one consultant who forced the issue with a C-Peptide... I would still be on insulin, and I would still firmly believe that I was a type 1 with a failed pancreas - all the data to hand would back it up - but it would be wrong.
and - understand - at that moment, I was a late onset Type 1 with a positive C-Peptide - I was in precisely the same position as you both.
I cannot - and am not - trying to diagnose you; but I cannot help but wonder how often what happened to me, is actually the case for others who did not benefit from a bolshy consultant who was not prepared to sit back and scratch her head, but instead re-diagnosed me. As you say - it's rare. I was even warned that it was rare and considered dangerous to re-diagnose a T1 as T2 for at least a year, simply due to the dangers of removing insulin unless you are 100% sure there is still an internal supply.
I'm not even saying that you are wrong - hell, you know your own body better than I can. But - you either have a complicated situation that baffles medical understanding ... or the initial diagnosis may be wrong and the answer is simple, as it was for me.
For me - normal C-Peptide = functioning pancreas = cannot be T1 - so go full effort into trying for remission, what do you have to lose. (provided you can do it safely, and I was convinced I could based on what I could see from my CGM).
Please understand - I'm in no way trying to be critical. It's really that for me - the entirety of the medical profession had me pegged for a lifetime of insulin - except one person. And I feel so lucky to have bumped into that one person.
When you say "I was LADA" you may have been considered (mistakenly) to be and treated as such, but you weren't physiologically LADA because you didn't have autoimmune destruction of the pancreas, that is the key point. Again, "I was a late onset Type 1 with a positive C-Peptide" you weren't T1, you were miscategorised as one so not the same situation. It's relatively easy to determine by doing the antibody test. If you are negative for all the antibodies it's extremely unlikely that you have T1. It seems that it's possible to be T2 an have GAD antibodies, but in my extensive research I have only found one paper that says this, so I think it is quite a fringe idea, and in any case would be rare and only with very low levels of antibodies.Again - I was diagnosed and treated as a late onset type 1 for a year -
I was LADA - and I could easily have had this same conversation the other way around. It's only in hindsight that I can say that I was actually T2. Indeed this is rare, but my point is - the response of the medical world was to give me the treatment appropriate for a T1 - insulin - and had it not been for one consultant who forced the issue with a C-Peptide... I would still be on insulin, and I would still firmly believe that I was a type 1 with a failed pancreas - all the data to hand would back it up - but it would be wrong.
and - understand - at that moment, I was a late onset Type 1 with a positive C-Peptide - I was in precisely the same position as you both.
I cannot - and am not - trying to diagnose you; but I cannot help but wonder how often what happened to me, is actually the case for others who did not benefit from a bolshy consultant who was not prepared to sit back and scratch her head, but instead re-diagnosed me. As you say - it's rare. I was even warned that it was rare and considered dangerous to re-diagnose a T1 as T2 for at least a year, simply due to the dangers of removing insulin unless you are 100% sure there is still an internal supply.
I'm not even saying that you are wrong - hell, you know your own body better than I can. But - you either have a complicated situation that baffles medical understanding ... or the initial diagnosis may be wrong and the answer is simple, as it was for me.
For me - normal C-Peptide = functioning pancreas = cannot be T1 - so go full effort into trying for remission, what do you have to lose. (provided you can do it safely, and I was convinced I could based on what I could see from my CGM).
Please understand - I'm in no way trying to be critical. It's really that for me - the entirety of the medical profession had me pegged for a lifetime of insulin - except one person. And I feel so lucky to have bumped into that one person.
I would love to be in your situation and actually T2, as that can be put in permanent remission, but the presence of antibodies means unfortunately that I'm not. Also as time has gone on I have seen that I'm not insulin resistant now. My remaining insulin production can cope with the reduced demands from the low carb diet without drugs, if I push it and and have more carbs it doesn't. Yes the normal C peptide was confusing to me for a long time, I think the explanation I gave before of fasting vs stimulated ranges explains this, and as I said doesn't apply to your case because you aren't T1 therefore the physiological process is quite different. Some people with classic T1 have very rapid destruction and need insulin immediately, others have a good remaining production which can last many years, the longest "honeymoon" I have heard of is 15 years. It's still a much reduced production compared to a normal person though, just enough to get by if very careful.
Yes 100% consultants and nurses can miss things and be wrong. The nurse I saw in the first month was horrible and arrogant, when I finally got to see the consultant 6 months later he couldn't answer many of my questions, just a smarmy "we don't have data on that" when he didn't know the answer. He did at least admit that there is a lot still not known about diabetes and there is a high degree of individual difference across all types. Surely in your case it would have been simple to re-diagnose, all the needed to do was the antibody test? They were very unsure when I decided to stop insulin after 4 weeks, I am glad now I didn't listen to their advice and proved them wrong!
Chris24Main
Well-Known Member
- Messages
- 1,024
- Type of diabetes
- I reversed my Type 2
- Treatment type
- Diet only
OK - thanks for being so open.
I think we're in very broad agreement.
For what it's worth, I got an antibody test on initial diagnosis, but only was told the results after about 8 months - and they were inconclusive. At the time I was clueless, and don't even recall the numbers - but I was told that there were 5 antibodies - 4 with tests and I was negative to 2 of them; so just not clear enough to be sure of anything. It was not considered safe to change treatment on that basis, and it was only in conjunction with the C-Peptide test that I was re-diagnosed. Very much not a simple thing though, and as I say, I do feel extremely lucky on that front.
But - I totally accept your central point - physiologically there is a difference.
There was a very strong assumption that my pancreas was going down either way, but I'm now totally focused on insulin resistance and mitochondrial health, so I can't really speak to insult to the pancreas. One thing I keep meaning to chase down - is why the β cells are affected and not the Glucagon producing α cells - or maybe they are too.. and also the evidence that many auto-immune conditions seem to respond to lowering inflammation that comes with lowering glucose and insulin resistance (well, more than that.. but these are all now points of interest, and I sound more like an interested enthusiast, not someone searching for better understanding of his own condition).
anyway - good luck and long may the honeymoon last..!!
I think we're in very broad agreement.
For what it's worth, I got an antibody test on initial diagnosis, but only was told the results after about 8 months - and they were inconclusive. At the time I was clueless, and don't even recall the numbers - but I was told that there were 5 antibodies - 4 with tests and I was negative to 2 of them; so just not clear enough to be sure of anything. It was not considered safe to change treatment on that basis, and it was only in conjunction with the C-Peptide test that I was re-diagnosed. Very much not a simple thing though, and as I say, I do feel extremely lucky on that front.
But - I totally accept your central point - physiologically there is a difference.
There was a very strong assumption that my pancreas was going down either way, but I'm now totally focused on insulin resistance and mitochondrial health, so I can't really speak to insult to the pancreas. One thing I keep meaning to chase down - is why the β cells are affected and not the Glucagon producing α cells - or maybe they are too.. and also the evidence that many auto-immune conditions seem to respond to lowering inflammation that comes with lowering glucose and insulin resistance (well, more than that.. but these are all now points of interest, and I sound more like an interested enthusiast, not someone searching for better understanding of his own condition).
anyway - good luck and long may the honeymoon last..!!
Antibodies usually give a clear answer, you may have had very low levels, which either means nothing or you are in the very early stages of it, but that in itself unlikely to cause significant change to blood sugar. I had this argument with my consultant, as I had a very high level of GAD antibodies (the usual one) but tiny levels of another, way below the level marked as positive on the results. He said that detectable antibodies means that you have 2 antibodies at play so confirming his T1 diagnosis, I pointed out that at such a low level studies show that plenty of people in the general population have that (and GAD) but don't have or ever get diabetes and it's not significant. He acknowledged that, but of course can't ever admit to being wrong!OK - thanks for being so open.
I think we're in very broad agreement.
For what it's worth, I got an antibody test on initial diagnosis, but only was told the results after about 8 months - and they were inconclusive. At the time I was clueless, and don't even recall the numbers - but I was told that there were 5 antibodies - 4 with tests and I was negative to 2 of them; so just not clear enough to be sure of anything. It was not considered safe to change treatment on that basis, and it was only in conjunction with the C-Peptide test that I was re-diagnosed. Very much not a simple thing though, and as I say, I do feel extremely lucky on that front.
But - I totally accept your central point - physiologically there is a difference.
There was a very strong assumption that my pancreas was going down either way, but I'm now totally focused on insulin resistance and mitochondrial health, so I can't really speak to insult to the pancreas. One thing I keep meaning to chase down - is why the β cells are affected and not the Glucagon producing α cells - or maybe they are too.. and also the evidence that many auto-immune conditions seem to respond to lowering inflammation that comes with lowering glucose and insulin resistance (well, more than that.. but these are all now points of interest, and I sound more like an interested enthusiast, not someone searching for better understanding of his own condition).
anyway - good luck and long may the honeymoon last..!!
I have researched beta cell preservation a lot. One thing I am taking which hopefully is making a difference is GABA. The GAD antibodies block the production of GABA, which is an amino acid essential to many features but also pancreatic function. I again asked the consultant, if the antibodies deplete the body of GABA leading to a dysfunctional pancreas, why can't you just take it to replace that? His usual answer of "we don't have data on that" meaning he didn't know. There are plenty of positive reports from animal studies and it is being studied in trials at the moment, but I thought I would get ahead of the game. One of the things it can do is convert alpha cells to beta cells, so those who say the T1 pancreas can't improve that's not entirely true, although by how much I don't know. Worth a try anyway. I don't know if it would have any benefit in T2.
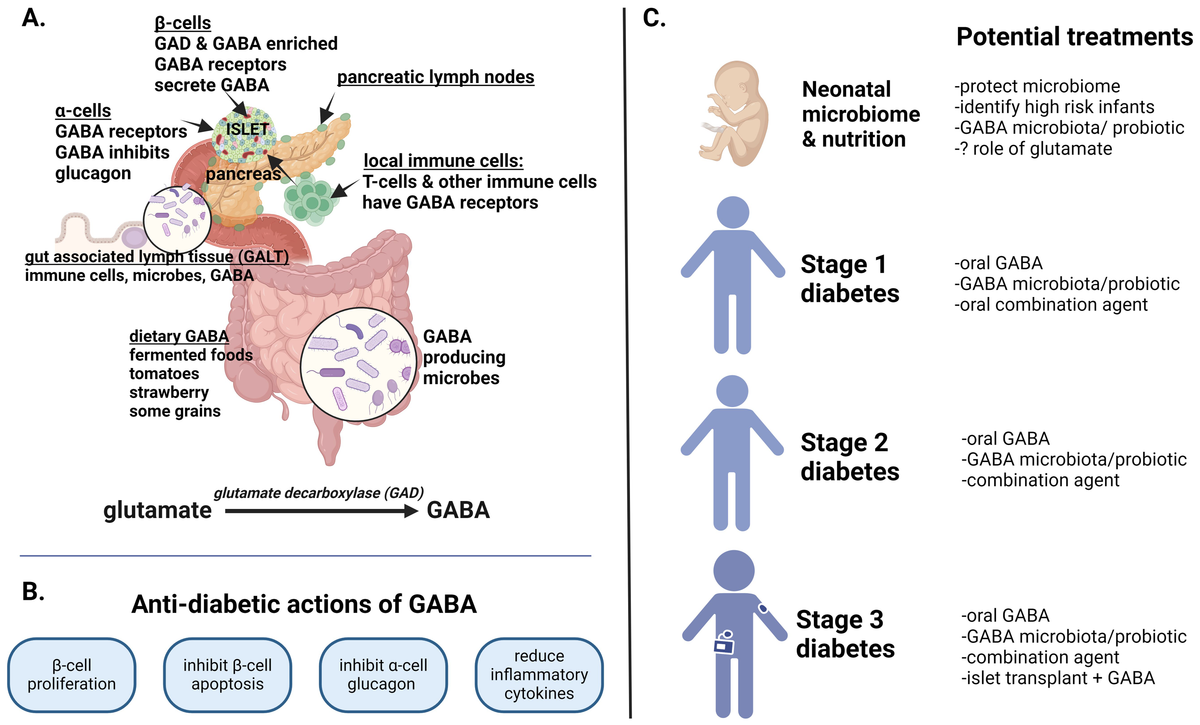
Frontiers | The role of GABA in type 1 diabetes
Gamma aminobutyric acid (GABA) is synthesized from glutamate by glutamic decarboxylase (GAD). The entero-pancreatic biology of GABA, which is produced by pan...
Yes, I agree @Vectian you. Certainly, when you have high titres of autoantibodies. In fact I suggested that your C-Peptide results were not that high (I believe they were around 1000 pmol/ls) given that your blood sugars were averaging 12mmol/ls back on May 30th 2024.See my last reply to LADA enigma, I think that explains how this can be (the same situation with me) and perhaps solves the enigma!
- Messages
- 10,406
- Location
- New Zealand
- Type of diabetes
- Type 1
- Treatment type
- Pump
- Dislikes
- hypos and forum bugs
While I appreciate that this remark is slightly off topic to a subject about LADA, am challenging this just because though it may well be true for some T2 it isn't for all. There are many different flavours of T2 and there are a number of reasons why a T2 might need insulin (eg long term reduction of endogenous insulin production, intolerance to other T2 meds). https://bpac.org.nz/2021/diabetes-insulin.aspxSo if you are T2 yes injecting insulin is definitely the wrong thing, the issue is too much insulin and therefore insulin resistance.
We were talking about just after diagnosis and trying to put it into remission, in that situation surely insulin would make things worse? My understanding is reduction in insulin production in T2 happens (if it does) much later after prolonged insulin resistance? C peptide scores are generally at or above normal range for T2s at diagnosis.While I appreciate that this remark is slightly off topic to a subject about LADA, am challenging this just because though it may well be true for some T2 it isn't for all. There are many different flavours of T2 and there are a number of reasons why a T2 might need insulin (eg long term reduction of endogenous insulin production, intolerance to other T2 meds). https://bpac.org.nz/2021/diabetes-insulin.aspx
Chris24Main
Well-Known Member
- Messages
- 1,024
- Type of diabetes
- I reversed my Type 2
- Treatment type
- Diet only
Hi @Vectian - Happy New Year and all.
I just wanted to pop in one last comment - thank you for your engagement on this; it's really helped me refine my thinking. What I need to constantly be aware of is that (as you actually pointed out) my diagnosis background is rare. Of course, LADA itself is quite rare to start with. You have clearly done a great deal of research, and this will stand you in good stead, whatever... but for many people, particularly with fresh diagnoses, this is all pretty overwhelming, and a high-level discussion can be intimidating, and I know in my enthusiasm, I can sometimes put things in a way that one detail or other can be interpreted in a way I hadn't intended (all of this gets ferociously complicated fast).
To kind of back up @EllieM on this - even in my case, I'm not 100% sure that the year of taking insulin didn't give my pancreas just the break it needed to recover to active duty. I just cannot know for sure. In many ways the answer to the OP is "it's complicated"...
I just wanted to pop in one last comment - thank you for your engagement on this; it's really helped me refine my thinking. What I need to constantly be aware of is that (as you actually pointed out) my diagnosis background is rare. Of course, LADA itself is quite rare to start with. You have clearly done a great deal of research, and this will stand you in good stead, whatever... but for many people, particularly with fresh diagnoses, this is all pretty overwhelming, and a high-level discussion can be intimidating, and I know in my enthusiasm, I can sometimes put things in a way that one detail or other can be interpreted in a way I hadn't intended (all of this gets ferociously complicated fast).
To kind of back up @EllieM on this - even in my case, I'm not 100% sure that the year of taking insulin didn't give my pancreas just the break it needed to recover to active duty. I just cannot know for sure. In many ways the answer to the OP is "it's complicated"...
Alexandra100
Well-Known Member
Are you sure? My understanding is that the patient has the right to ask to be referred for free to another NHS doctor or specialist. (Or to a private one, but then you have to pay.) I got myself referred to a specialist recommended by someone on here. He practised in London and somewhere else far away, so we talked on the telephone. I wasn't actually that impressed - we were not a match made in heaven - but I was glad I tried.All the GP can do is refer me back to the diabetes centre at my hospital, where I'm already registered. So I end up with the same nurse, who says that because you are GAD positive you automatically have T1, with no discussion.
