D
Deleted member 388305
Guest
Thanks for your response Mbaker!Well done on getting into the remission range and posting some results. This makes the contrast so far almost perfectly between the low caliorie high carb method for others. What were your results on low carb.
Over the years, I maintained an A1c between 6.0 and 7.0 most of the time, but could never get below 6.0 no matter how few carbs I ate. That said, I found it increasingly difficult to do. I wasn't getting the results I used to get, which in turn made it more difficult to stay on the eating plan. This is over a 20 year span of time. During COVID, the wheels came off so I was looking for something to motivate me to do better. A doctor recommended I consider this and sent me a link to a video by the Mastering Diabetes guys. I spent three days reading their book and decided it made sense enough to give it a shot. If it is true that abdominal and dietary fat cause insulin resistance, then it makes sense that the harder I worked at low carb (meaning essentially that the fat percentage of my diet became higher over time), then the more insulin resistant I was making myself.
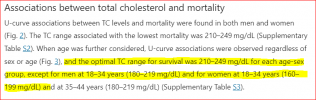
Are you familiar with the work of Dr. Caldwell Esselstyn? He treats heart patients with this diet. He says that if you are eating this way and achieve a Total Cholesterol of <150 and an LDL of <80, then any heart disease you have will not progress and in very many cases will reverse. So he doesn't view HDL as being so important in that case. I have read elsewhere that not all HDL is "good." Here is a link to a Caldwell TED Talk.Not a criticism as we are all using hypothesis, but your trigs are "better" than average (according to modern ways of reviewing lipids), howver they are 33% more in absolute terms more than mine - more fat in the blood on a low fat diet than someone eating lots of fat. The HDL of 0.85 is below both US and UK standards and compares to my latest a couple of weeks ago of 2.9, whilst your LDL is over 2 times lower than mine (so on modern metrics better). So on lipids a traditional Doctor would say LDL trumps everything making yours better. The low carb Doctors would favour mine as being more protective.
Making Heart Attacks History.
Here are my Medichecks tests a few months ago, which show a similar A1c to yours and a very low HS-CRP of 0.3:
I got my HS-CRP lab report a few minutes ago and mine was 2.0.
apolipoprotein B 74
Mostly I walk, pretty much every day - usually between 1.5 and 3 miles. I ordered some dumbbells which should arrive today and hope to add some muscle to further improve my glucose uptake. I also do Tai Chi. The Tai Chi and walking sort of take up the same time spectrum; if I do more of one then I do less of the other.View attachment 57193
To round this out can you post typical meals on your protocol and if you do exercise, what is it, here are some of my meals this week:
I don't have any food pictures, but I can give you an idea of what I eat.View attachment 57190
View attachment 57191 View attachment 57192
I am hoping you send your exercise (if any), hs-crp, typical meals and indication of your post-prandial readings (mine 1.7 mmol/mol); people can make an assessment as to which protocol suits them more, essentially do they believe in the high LDL kills you hypothesis or low HDL and higher Trigs does and plant or animal based food preferences. Whilst this is an oversimplification some of the big ticket items are addressed.
For breakfast I typically eat steel-cut oatmeal with 1/2 a banana, blueberries, cinnamon and flax seed with black coffee.
At some time during the day I will eat a large sald - either at lunch or dinner, but most often at lunch: In addition to whatever greens I use, I will add half a cup or more of beans, some tomatoes, peppers, cumin, vinaigrette. This is usually followed by a large plate of vegetables which can include green beans, sweet potatoes, squash, carrots, etc., etc. and an apple. I may also have a serving of brown rice or quinoa or more beans topped with another half a banana and blueberries.
Mid-afternoon I have a smoothie which includes frozen fruit, kale, broccoli, flax seed and plant protein powder. I have a slice of Ezekiel Bread with it.
If I have eaten all the above, then at dinner I will probably just eat a serving of raw unsalted nuts (almonds, cashews or walnuts) a square of 85% dark chocolate and perhaps another apple.
We have just now started exploring recipes so have added a couple of good ones - one for a soup containing potatoes, lima beans, asparagus and leeks as well as one for ratatouille.
Hope this helps. Anyone who has any interest in this really needs to carefully read the book and check out the references to the relevant studies. Also, remember this is a process and I am only into it 6 months. These results are better than they were 3 months ago and I expect more changes in the days ahead.
Last edited by a moderator: