Hi @Drfaxan,
Interesting question and sure one which most of us T2s have pondered on at one time or another. Personally, I've read some on this topic (some sources providing contradictory information as is so often the case in science) and have been pondering on why some of us become T2 (and others not).
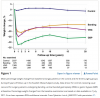
Have you seen this graph by Dr. Ken Sikaris, a chemial pathologist, which shows that insulin levels on average are higher for people with diabetes than normal people? This even holds true for people with very high HbA1cs. It should also be mentionend that this graph includes Type 1s with no to very low insulin production -- just the results of all tests coming in to a clinical lab from various sources.
So looking at this, imo there is not necessarily a deficit of insulin in the majority of T2s (some might even argue the reverse is true especially for HbA1cs in the prediabetic range).
So, maybe one of the primary defects in T2 (at least for some) is not a lack of insulin or pancreas burnout? Then maybe the problem is somewhere else? Some evidence seems to point at a fatty liver instead. Some researchers have observed that a fatty liver keeps churning out glucose as it no longer responds to insulin, which would normally inhibit glucose production. So, if we eat (especially carbs) glucose increases, insulin increases, however as the liver doesn't surpress glucose production, this glucose is then added to the glucose coming from food and blood sugars increase way above what would be normal (and leading in turn to more insulin secretion). So, if we subsequently eat carbs throughout the day by having several small meals in a day and/or by constant snacking, insulin is elevated throughout the day (and thus preventing us from burning fat -- fat burning can only occur when insulin is lowish). Because insulin is constantly needed to control blood sugars, this might also prevent us from building an insulin store needed for the first-phase insulin response when we eat (a lacking or low first-phase insulin response is also often a defect in T2s).
If this is really one of the primary mechanisms of blood glucose disregulation in T2, measures which reduce constant production of insulin should help many of us, this includes low-carb/keto, fasting, low calorie, and/or exercise (facilitating non-insulin mediated glucose uptake). Consequently, allowing us (and our livers especially) to shed fat -- and some research seems to suggest that the liver is from where we first lose fat when insulin levels drop -- might mean that we are actually acting on one of the root causes of T2. The flipside of the coin then potentially is that medications increasing insulin levels for T2s (by giving sulfonyureas and insulin) might make the problem worse for probably many of us. This is why I believe that measuring insulin production in all newly diagnosed diabetics is absolutely essential before deciding on treatment.
Coming back to your question -- yes reversal (or even cure) might be possible, though some are more comfortable with the term control. It also implies if we go back to our old way of eating, we might be reversing the reversal. No matter what you choose to name this, the important fact is that we are minimizing chances of complications when we normalize metabolic processes (even when we use appropriate medications for this).
By the way, I recently listened to a podcast by Peter Attia and Gerald Shulman. An interesting fact mentioned was that in a study of college kids at the age of 20 and no weight problems, insulin resistance was already present in about half of them. Also, some studies show that descendents of T2 diabetics already seem to have some insulin resistance in childhood. This seems to suggest that genetics play a large role (though I might not really want to call it a defect when it affects so many people) and the problem arises when this genetic makeup interacts with the modern food environment.
Not sure whether this answers your original question. Just trying to think through some of what I've read and listened to in the last few years.