Hi Sean thanks for your gracious post.
My medical history started the day I was born. But that is a very long story.
Poverty covered my school years, hunger was a bad friend.
I was always told to eat what was put in front of me. But I couldn't.
The dairy intolerance was evident from childhood, I was ill often with nausea and diahorrea. And butter would have me vomiting, milk would bloat me, it seems that sterilized milk was better than pasteurised. The lactose intolerance is in my family and in my close family, an uncle, an aunty, my niece, my grandson. But all the others are not. I have been told that.it having butter or spread on a sandwich is so unusual, the question is asked, what do you have instead? Nothing!
Cooked vegetables especially the greens, I couldn't eat, my taste buds wouldn't allow it, so I was often in trouble at school for not eating, cabbage, sprouts, carrots, turnips, cauliflower and spinach, but I could eat the carrots and spinach as pert of a salad with lettuce, toms, cucumber etc. That is how I get my veg micronutrients.
I enjoyed my junior school, swimming, football, cricket and others who like me, there only real food was school dinners. But home life was hard, not much room, lots of chores because my mum worked but my dad had malaria twice and was only able to do light work, but his health was very poor, heart and low blood pressure.
Grammar school wasn't any better, like a fish out of water. Yes, I passed my 11+
But the grammar school was beyond my social class. We were tolerated to some degree but it was really bad. As a school.
Typically I was a very good sportsman, and I played representative cricket at the age of nine and ten for my local area. I was probably the best cricketer in the school, but because of my class, I didn't get picked until my last year, I never made the football, swimming, rugby team even the chess team was no go.
You knew what you were and the posh kids told you. The master's were worse.
So I really had a bad start to life, but it never deterred from bettering myself.
I got a couple of A levels in history and art, how I don't know. I got o levels in geography, maths, chemistry, English.
I wanted to be a machine printer, I passed the test and IQ test, to get my apprenticeship but could not find a firm to take me on. So the day I finished school, the next day, I got a job as a do everything that happens in a printing company.
I was there for two years, before going onto a car manufacturer. I spent 35 years there. Until 2007.
I was doing shifts, eating or not at stupid o'clock, lots of rubbish, white bread, , and after I married, helping out to feed four kids and yourself, so convenient food and a rubbish diet, I was still quite fit because of walking, on my feet at work and at home.
I was a team leader and supervision over thirty men at times. My job was stressful but there was so many good times.
So you could say that I worked my way to a decent job, improved my life and started getting the benefits of a family life with little monetary issues.
During my last ten years I got abroad through my job and visited plants in Germany, Belgium, France and Spain. I was also down south with engineering on pilot.
I got interested in electric powered vehicles and worked on a prototype electric vehicle, but it was too heavy to be a production car. The battery life was poor and too big and heavy. The transformation in the last twenty five years has been unbelievable.
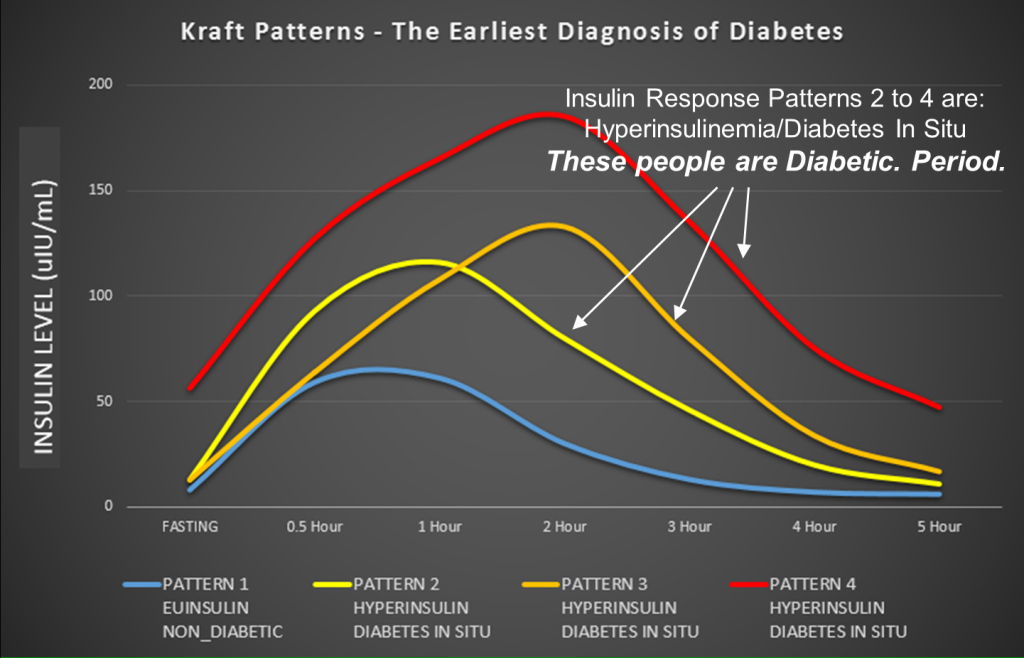
So I retired, and I was already under my doctors due to my issues with my stomach problems, hence the heliocobacter pylori infection was part, that was when my battles with the medical profession started, as described in my last post, they were just following the usual dietary advice. If I had a insulin test instead of the usual blood panel done then, I am convinced that my hypo hell might not have happened.
But I was getting symptoms akin to a metabolism problem, the doctors never took it seriously, especially after my first endocrinologist dismissed me. The one thing I repeated every time was I'm not eating a lot and I'm working, walking all day, and I'm getting heavier. So because I was down on my medical history as prediabetic, T2, not one of the doctors listened or even thought of getting me an endocrinologist. They were dismissive about my symptoms and didn't believe my intake, no alcohol and my lifestyle. I did get in a bit of a kerfuffal with one of the receptionists. But I had to apologise, to see my doctor again.
So as my symptoms were increasing, my impatient followed, and a lot of what happened during these years is missing, even some important celebrations, and Christmas. There was quite a few deaths in the family, within five years, I lost my mother (I was on death watch for a total of ten days, she was in a coma) and two brothers, one to cancer and the other to a massive coronary. The wife lost her mother and also two brothers since. I was getting bigger and heavier and my health was going downhill fast.
I could only work part time and it was a struggle, I had a few incidents that required hospital treatment and even one blood finger prick test read normal. So nothing was said.
Yes, very tough especially frustrating because I didn't have a clue what was happening to me.
So since diagnosis and losing all the weight I put on, within two years my health returned, all my organs were good, all my symptoms mainly went away, no insulin resistance and because I wasn't on the hypo rollercoaster, my hyperinsulinaemia cured itself. My NAFL went, my function results were normal. My fasting bloods were normal, my Hba1c levels were normal, my cholesterol came back at around 4 in total.
For a man of my age and gone through all my troubles, with the family history of heart problems, mine came back normal. Go figure?
My specialist endocrinologist who always smiled when in consultation and was shocked at my weight loss. This began the drug tests and more glucose tolerance tests.
So, no incretins, and yes, secondary insulin is the overshoot. So, yes, it is the insulin that drives me into hypo and yes, the only other way to boost glucose levels is to eat, that is why it is recommended to eat every three hours. But that is unnecessary if you don't eat carbs. And because of no carbs it doesn't trigger a spike, and no insulin overshoot, no hypo! And more importantly, not many symptoms. And also the threat of going hypo overnight. Staying in normal range of blood levels works.
Yes, by a look at reactive hypoglycaemia, there isn't a lot of research especially in this country, I have read papers from the USA and other countries.
I have scoured the internet, Wikipedia is reasonably accurate and some good information there.
This is why, I had to find out about how my weird body worked, my new GP in 2013, labelled me so and my specialist endocrinologist confirmed this when having a humorous moment.
Thanks again, it is a good thing that we learn about others and not fall into the trap of lumping every one into labels of conditions. Every one is different, fingerprints, eyes, gut bacteria, even our response to life, why is there so many different side effects from certain drugs and not everyone?