Nocturnal hypoglycemia or night time hypos are common in people who treat their diabetes with insulin. Symptoms are usually only realised once waking up from a hypo.
Due to their nature, you will usually only find out about having a hypo during the night after waking up from a hypo.
Therefore people may not even be aware that they are having night time hypos, so it’s useful to be able to spot the signs and symptoms of when nocturnal hypoglycemia may be taking place.
Whilst nocturnal hypoglycemia is most common in insulin users, it can also occur for people who take oral anti-diabetic drugs.
Symptoms of night time hypoglycemia
Sometimes you may wake during an episode of nocturnal hypoglycemia.
However, if you don’t, you may notice one or more of the following indications that hypoglycemia may have occurred whilst you were asleep.
- Waking with a headache
- Experiencing seemingly unprovoked sleep disturbance
- Feeling unusually tired
- Waking with damp bed clothes and sheets from sweating
Having a clammy neck can be a particular indication of night time hypoglycemia.
Nocturnal hypoglycemia in children
For parents of children with diabetes, nocturnal hypoglycemia can be particularly worrying.
Parents of diabetic children may wish to check their child’s neck whilst they are sleeping if they are worried that night time hypoglycemia may be occurring.
Causes of nocturnal hypoglycemia
The chances of having night time hypos may be increased by the following:
- Too high a level of basal (background) insulin
- Physical activity during the day can increase insulin sensitivity which can lead to night time hypoglycemia, particularly for the first night after a sustained session of activity
- Following alcohol consumption
- Absence of a night time snack when one is usually taken
- Missing out dinner
- Following a period of illness if basal insulin was increased
Treating night time hypos
The treatment for night time hypos is the same as the general advice for treating hypos
That is to take 10 to 15g of a quick acting sugary food (such as sweets or glucose tablets) and some slower acting carbohydrate such as a slice of bread to prevent a further hypo taking place.
Have some quick acting carbohydrate next to your bed so that if a hypo occurs, you can treat it as quickly as possible.
Preventing night time hypoglycemia
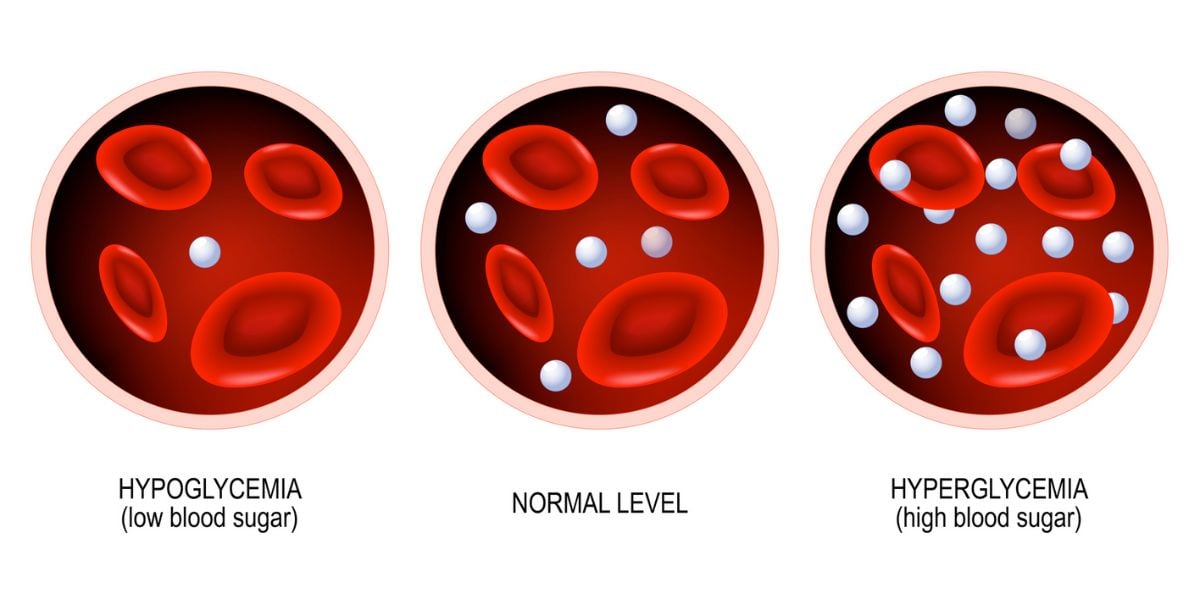
A useful first step towards preventing hypoglycemia is to test your blood glucose levels before bed.
For people on two or more insulin injections per day can help prevent hypos over night keeping blood glucose levels above 6.5 mmol/l before going to bed.
If over night hypos are suspected, carry out a test at 3am. Together with a before bed and first thing in the morning test, this can help to understand how your sugar levels are behaving over night.
If sugar levels are dropping too low over night, you may need to adjust your insulin doses. Speak to your doctor if you need help with correctly adjusting your insulin
The other way to prevent sugar levels going too low is to take some carbohydrate before bed.
Hypos can also be prevented by:
- Ensuring you basal insulin dose is not too high
- Reducing your night time/evening long acting insulin following exercise
- Taking carbohydrate before bed following an evening/night of drinking
- Not missing out dinner or any snacks you would usually have
Concerned about hypos? Join the (free) Hypo Awareness Program for a comprehensive guide towards improving hypo awareness »