Whether you are going on holiday or simply spending some time outdoors in the heat, hot weather and close humidity can affect people living with diabetes.
Increased heat does affect some people with diabetes, and with heatwaves becoming increasingly commonplace across the globe, it is even more vital that you know the precautions to take and signs to watch out for when keeping safe.
What problems can hot weather cause for people with diabetes?
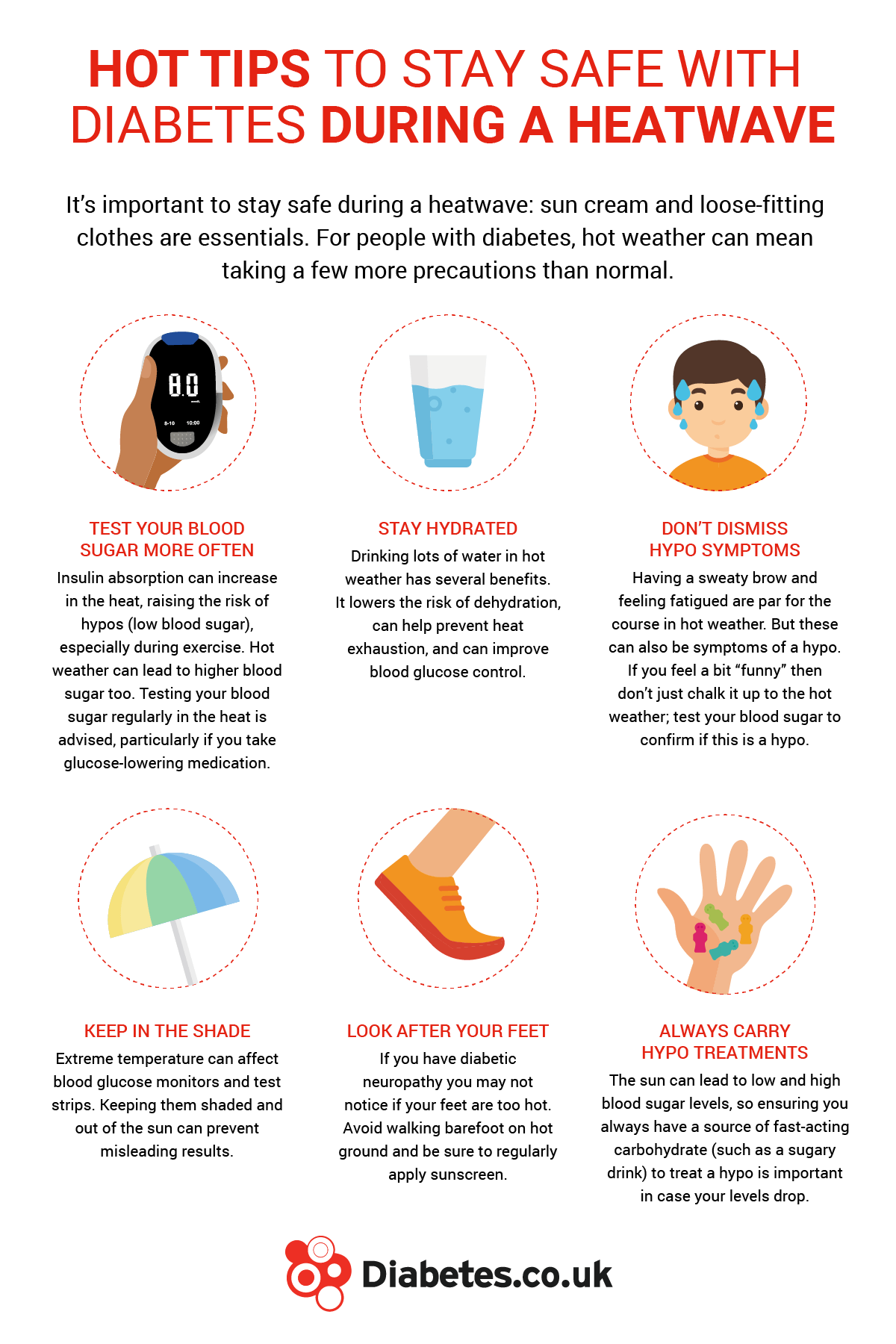
Dehydration can be an issue in hot weather, and higher blood glucose levels can further increase this risk.
People with diabetes should increase their intake of fluids in warm conditions by drinking water regularly throughout the day, compensating for what is lost as the body attempts to cool itself down through sweating.
One of the major concerns regarding diabetes and hot weather is the risk of blood sugar levels rising or falling and causing hypoglycemia or hyperglycemia.
What are the hypo risks from hot weather?
Hot weather can increase the risk of hypoglycemia for those on blood glucose-lowering medication such as insulin.
The body’s metabolism is higher in hot and humid weather, leading to an increased chance of hypoglycemia as insulin absorption increases.
Hypos may be slightly harder to spot in hot weather. Don’t be tempted to disregard hypo symptoms, such as sweating and tiredness, as a result of high temperatures as it could be a sign of hypoglycemia.
Find out more about spotting symptoms of a hypo here.

Take extra care if you’re driving. Test your blood sugar before and after each journey, and stop regularly to check your blood sugar during longer trips.
To prevent hypos, be prepared to test your blood glucose more often, particularly if participating in physical activity in hot weather. Keep a source of fast-acting carbohydrate at hand, such as glucose tablets or a sugary drink.
You may need to adjust your insulin levels during temperature changes. If you are experiencing higher or lower blood sugar levels and need advice about adjusting your insulin levels, speak with a member of your healthcare team.
What are the symptoms of heat exhaustion?
The NHS notes that people with diabetes are at higher risk for heat exhaustion. Heat exhaustion occurs when your body becomes overly heated and finds difficulty in maintaining or adjusting its temperature. Being overweight or obese may also make it harder for the body to cool down.
Symptoms of heat exhaustion include:
- Sweating more than usual
- Body temperature of 38°C or above
- Dizziness
- Cramping muscles
- Clammy skin
- Headaches
- Fast heartbeat and
- Nausea
By resting away from the glare of the sun and drinking more water you can avoid heat exhaustion. The symptoms you experience are the body’s signals telling you to lower your body temperature.
If you, or someone you know is suffering from heat exhaustion:
- Drink water or sports drinks to rehydrate
- Rest in a cool place – ideally with shade, fan or air conditioning
- Remove tight-fitting and/or clothing that is not required
- Expose as much skin as possible
- Cool your skin – ideally with cool water, spray, cold packs or wet sponge
- Fan your skin while wet to help your skin cool down
How can I tell the difference between heat exhaustion and heatstroke?
Signs of heatstroke include:
- Persistently feeling unwell after resting in a cool place and hydrating
- Not sweating even when you are feeling too hot
- Body temperature of 40°C or above
- Seizures
- Loss of consciousness or lack of responsiveness
Heatstroke happens when the body can no longer regulate the heat, causing the core body temperature to elevate dangerously.
If someone is showing signs of heatstroke, call an ambulance.
What about hot weather and medicine?
The heat of summer can be a problem when carrying diabetes supplies that need to be kept cool, such as insulin.
Get around this by keeping your medication away from direct sunlight and carrying cooling packs, which keep medicine cool.
Test strips are sensitive to temperature as well. Test your blood sugar in a cool, shaded place and keep your test strips away from direct sunlight as well.
Going travelling?
There are several other factors you’ll need to consider if you’re going away, such as time zone differences and the effects of long-haul travel. Read more about travelling with diabetes here.