Inflammation is a term often associated with long-term conditions like diabetes. Learn about what inflammation is and how it can impact people with both type 1 and type 2 diabetes.
What is inflammation?
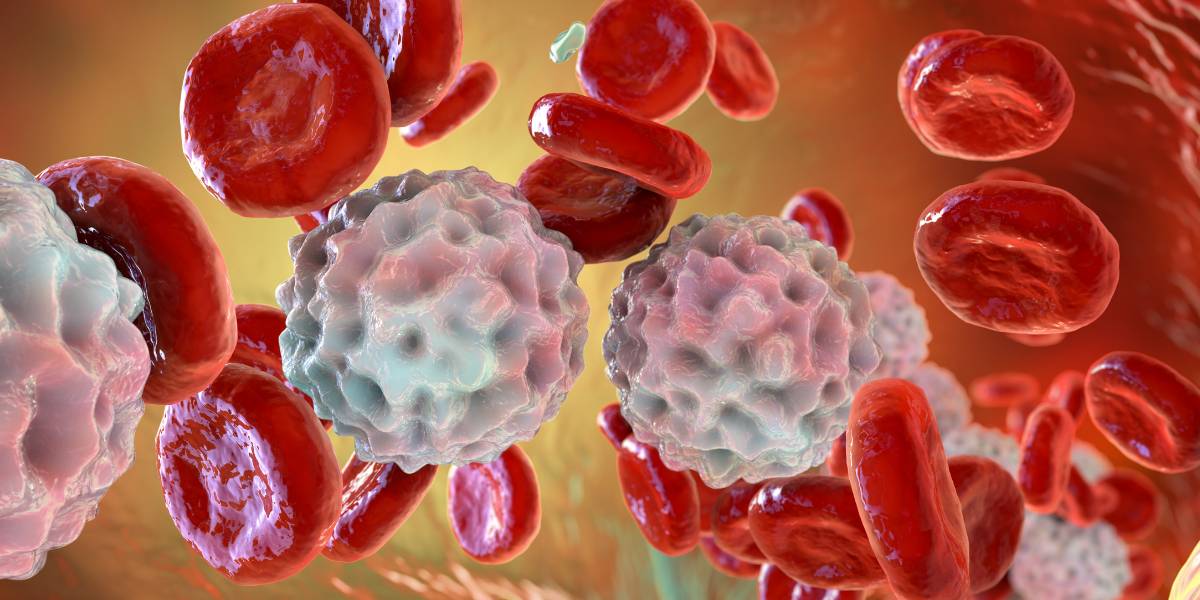
Inflammation refers to the immune system’s defence mechanism against harm or infections. Whenever the human body recognises threats such as pathogens, cell damage or irritants, it activates a protective biological response which involves widening blood vessels to enhance blood flow and summoning immune cells to the scene for healing.
Inflammation is classified as either acute or chronic.
Acute inflammation
Acute inflammation is the body’s immediate reaction to harm or infection which manifests with symptoms including redness, warmth, swelling, pain, and sometimes temporary loss of function. Once the root cause of acute inflammation is addressed, inflammation typically subsides.
Common instances of acute inflammation include:
- Inflammation in the airways due to acute bronchitis
- Sore throat caused by a flu
- A bee sting
- Physical injuries such as a broken toe
- Minor skin wounds
Chronic inflammation
Chornic inflammation refers to the prolonged inflammatory response that can last from months to years which arises when the body can’t remove the root cause of inflammation or when a subtle response persists without a clear reason.
Chronic inflammatory conditions include:
- Rheumatoid arthritis
- Asthma which can cause inflamed air passages
- Periodontitis
- Crohn’s disease
- Eczema
What causes inflammation?
Inflammation can be triggered by a number of things – from external injuries to internal autoimmune disorders.
Chronic inflammation is also often a byproduct of lifestyle choices such as:
Obesity can also induce persistent mild inflammation.
What are the symptoms of inflammation?
Recognising the signs of inflammation can enable treatment and/or intervention.
Common signs of inflammation include:
- Redness: An inflamed area often appears redder than the surrounding skin due to increased blood flow.
- Heat: The inflamed region may feel warm to the touch, again due to enhanced blood circulation.
- Swelling: Fluids and immune cells accumulate in the inflamed area, leading to noticeable swelling.
- Pain: Inflammation often causes discomfort or pain, especially when the inflamed area is touched or moved.
- Loss of function: In some cases, the inflamed part may not function optimally. For instance, an inflamed joint might restrict movement.
Consult a healthcare professional if you notice persistent signs of inflammation, especially if they’re accompanied by other symptoms like fatigue, fever, or unexplained weight loss.
What are the risks of inflammation?
Short-term inflammation is protective but long-term, chronic inflammation can be hazardous to the body.
Over time, it can harm healthy cells and tissues and is linked to several conditions associated with diabetes including cardiovascular disease, neuropathy, retinopathy and nephropathy.
What’s the link between diabetes and inflammation?
Both type 1 diabetes and type 2 diabetes have inflammatory components.
Type 1 diabetes occurs when the body mistakenly attacks the body’s beta cells which produce insulin after an inflammatory process in people with a genetic disposition for the condition.
In type 2 diabetes, the body becomes resistant to insulin, meaning it can’t use insulin effectively and over time, the pancreas can’t produce enough insulin to keep blood sugar levels in control.
While the exact cause of insulin resistance isn’t fully understood, inflammation plays a significant role.
Fat cells, especially in people who are overweight or obese, release pro-inflammatory chemicals called cytokines which can disrupt the action of insulin in cells.
In people with type 2 diabetes, inflammatory markers such as C-reactive protein (CRP) may be elevated even in the absence of an infection or injury.
Persistent inflammation can damage tissues over time and contribute to the complications of long-term high blood glucose levels.
How can I minimise inflammation?
Research has shown that chronic inflammation can be improved through:
- Eating a healthy diet: A diet rich in low-carbohydrate fruits, veggies, lean meats, healthy fats, and grains have anti-inflammatory components like omega-3s, antioxidants, and fibre.
- Keep blood sugar levels in range: High blood sugar levels can lead to the oxidation of free fatty acids in your fat cells, further promoting inflammation.
- Being active: Aerobic exercise can help combat chronic inflammation.
- Stress: Research shows stress can cause inflammation. Try mindfulness, meditation, and yoga to reduce stress levels.
- Getting sleep: Lack of sleep is associated with inflammation.
- Limit smoking: Nicotine activates white blood cells called neutrophils which cause increased inflammation.
- Limit alcohol: Alcohol can promote intestinal inflammation.