A report which gathered the data from cases of the novel coronavirus (COVID-19) outbreak in China was published by the Chinese Center for Disease Control and Prevention (China CDC). This report detailed the characteristics and patterns of 72,314 COVID-19 cases that had occurred in China, as of 11 February 2020. [1]
A review and summary of the findings of this report, titled Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China, was published on 24 February 2020 by the Journal of the American Medical Association (JAMA). [2]
This review summarises and emphasises the key findings and lessons from the cases from China. The key findings are broken down to:
- Patterns and outcomes of the COVID-19 cases (epidemiologic characteristics)
- Comparisons with previous viral outbreaks
- The response and learnings
Patterns and outcomes of the COVID-19 cases
Table 1 shows the breakdown and outcomes of the cases recorded. Out of the 72,314 cases, 62% of these were confirmed cases, where the patient tested positive from throat swab samples. 22% were suspected cases, where the diagnosis was based on the patient’s symptoms, 15% were diagnosed cases, where the diagnosis was based on the patient’s symptoms – this was used for the Hubei province only, and 1% of these were asymptomatic cases, where the patient tested positive but lacked the typical symptoms.
The age breakdown of the cases can be seen in Table 1, mostly grouped in the 30-79 age range.
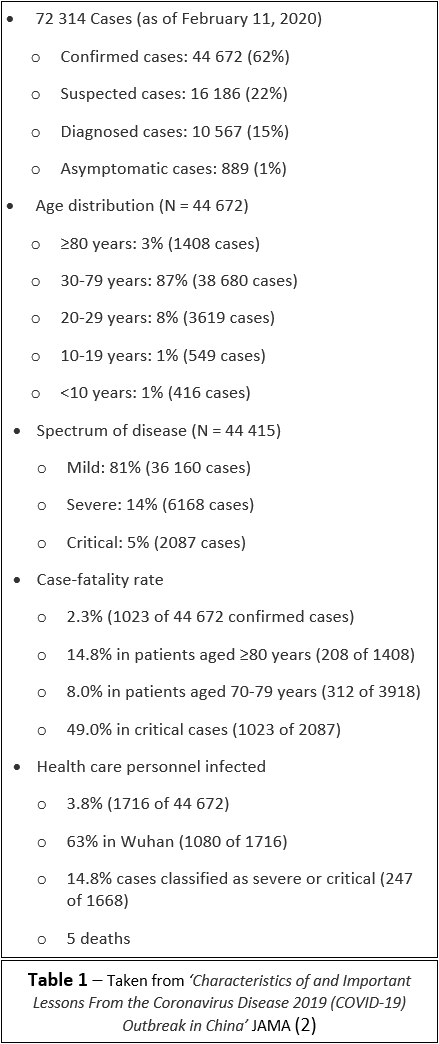
Most of the cases recorded were mild cases (81%) where the patients developed mild symptoms such as a cough or sore throat or only mild pneumonia, a lung infection where the alveoli (air sacs in the lungs) are inflamed.
14% of the cases were severe which meant the patients developed more serious pneumonia or lung infection. This could mean the alveoli in the lungs filling with mucus or fluid making it harder for the body to take in oxygen causing dyspnoea (shortness of breath) or difficulty breathing.
5% of the cases recorded were critical, which meant that the patients developed respiratory failure (when the lungs can’t get enough oxygen), septic shock (where the infection spreads throughout the body), and/or organ failure.
The overall death rate from the cases recorded was 2.3%. Elderly patients and those with underlying health conditions were more likely to be more seriously affected. The death rate changed depending on the age group, which ranged from 0 deaths in the under 9-year olds, to a 14% death rate in those aged over 80 years. Those with underlying health conditions such as heart disease, diabetes, cancer and lung disease had higher death rates reported. [2]
The virus also rapidly spread from a single city of Wuhan to the entire country in 30 days overwhelming the healthcare system. [1,2]
COMPARISONS WITH PREVIOUS VIRAL OUTBREAKS
The JAMA review looks at the comparisons between the COVID-19 outbreak in China and 2 previous viral outbreaks. These are the Severe Acute Respiratory Syndrome (SARS) from 2002 to 2003 and Middle East Respiratory Syndrome (MERS) from 2012 which is ongoing [2].
Similarities:
- Both SARS and MERS can be traced to zoonotic transmission (when a pathogen such as a virus is passed from an animal to human). These were both novel coronaviruses, the same as COVID-19.
- All 3 of these viruses cause similar symptoms such as a cough and lung infections and affected the elderly and those with underlying health conditions more seriously
- Testing involved throat swabs to extract nucleic acid, which holds the virus’ genome (genetic material)
The main differences observed so far are the death rates appear higher for both SARS (9.6%) and MERS (34.4%), according to the World Health Organisation (WHO), than the current data suggests for COVID-19 (at 2.3%). However, COVID-19 has caused many more deaths due to the larger number of cases. The JAMA review suggests that the case number may even be higher than recorded due to the difficulty in testing the population and also identifying and counting those cases which may not develop any symptoms [2,3]. Further research and data collection is required to fully understand the death rate for COVID-19.
The current data from the report from China CDC suggests that COVID-19 is more transmissible or easily spread than SARS or MERS, where transmission often occurred in hospital when the patients were being treated [1]. The data for COVID-19 suggests virus transmission is occurring in hospitals, as cases are being seen in health workers, however more cases are spreading in the community and in households. 64% of clusters (cases closely grouped in time and place) documented have been in family households (data from the Chinese Center for Disease Control and Prevention presentation made to the WHO Assessment Team on 16 February 2020). However, the JAMA review concludes that more research is still needed to determine exactly at what rate COVID-19 is spreading. [2]
Response and learnings
The JAMA review also looks at how the Chinese government responded to COVID-19. In comparison to the SARS outbreak in 2002, the WHO was notified of the outbreak much earlier for COVID-19. [2]
The initial Chinese government response was focused on isolating and quarantining the cases, social distancing and community containment (lockdown measures). Large gatherings were cancelled, and travel restricted around the country. [1]
These approaches aimed at reducing infections and deaths have also caused economic damage to the country. There have been questions if these potential benefits outweighed the costs, however more and more countries around the world have had outbreaks since and enforced similar measures to China. [4,5]
A goal of the responses enforced by the Chinese government was to buy more time for more research and data to be collected on this new disease. The report of the cases published by the Chinese CDC was to help inform health workers in other countries dealing with COVID-19 of the characteristics and patterns [1]. As the rest of the world deals with the spread of COVID-19, more evidence is emerging every day which can help to inform the tactics governments and health workers need to follow in responding to this pandemic.
Read more:
- A general guide to diabetes and coronavirus
- Coronavirus: should I be worried
- Update for those vulnerable to Coronavirus
- Dr Dipesh Patel on diabetes and vulnerability to COVID-19
- Rhonda Green: Working on the frontline with type 1 diabetes
- Laura Thornton: a diabetes hero on the Coronavirus frontline
- Grandad with diabetes recovers from COVID-19
References:
[1] Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly. [Online] Available at: http://weekly.chinacdc.cn/en/article/id/e53946e2-c6c4-41e9-9a9b-fea8db1a8f51 [Accessed 24 April, 2020]
[2] Wu Z , McGoogan J M (2020). Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China. JAMA. [Online] 2020;323(13):1239-1242. Available at: https://jamanetwork.com/journals/jama/article-abstract/2762130 [Accessed 24 April, 2020]
[3] Battegay M , Kuehl R , Tschudin-Sutter S , Hirsch HH , Widmer AF , Neher RA (2020) . 2019-Novel coronavirus (2019-nCoV): estimating the case fatality rate: a word of caution. Swiss Med Wkly.[online] 2020;150:w20203. Available at: 4414/smw.2020.20203 [Accessed 24 April, 2020]
[4] Lacobucci, G (2020). Covid-19: UK lockdown is “crucial” to saving lives, say doctors and scientists. BMJ. [online] 2020; 368. Available at: https://doi.org/10.1136/bmj.m1204 [Accessed 24 April, 2020]
[5] Lazzerini M, Putoto G (2020). COVID-19 in Italy: momentous decisions and many uncertainties. The Lancet. [online] Available at: https://doi.org/10.1016/S2214-109X(20)30110-8 [Accessed 24 April, 2020]





