A new study has found that people using a digital weight-loss app alongside specialist obesity care lost more weight, improved their blood sugar control and reported better quality of life than those receiving clinic care alone.
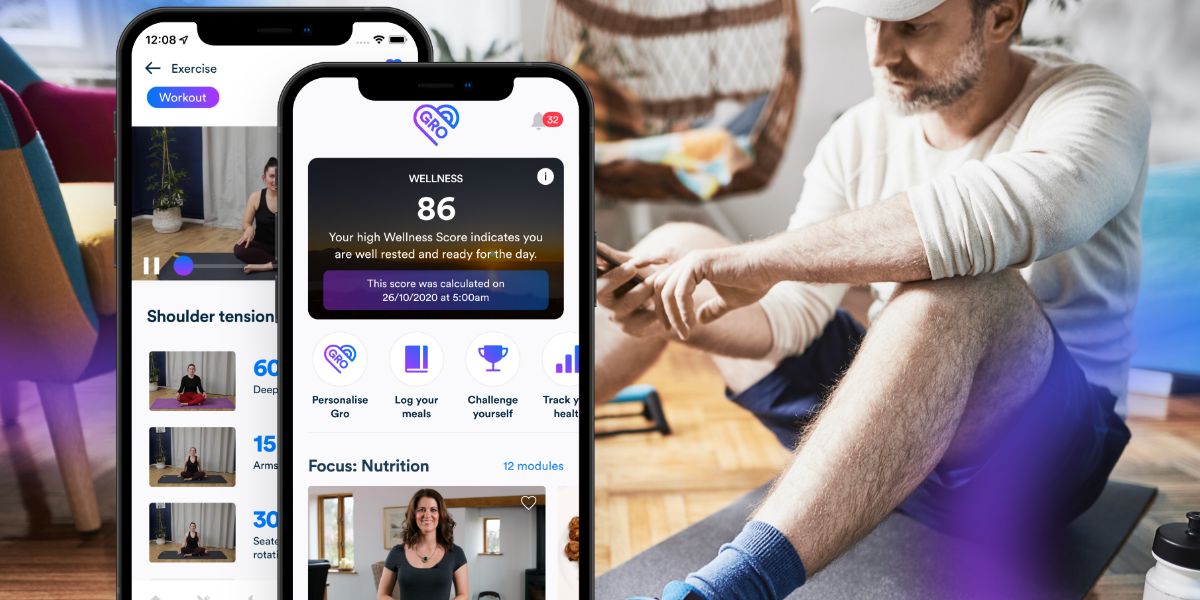
The research, published in the Journal of Medical Internet Research, evaluated Gro Health W8Buddy, a smartphone and web-based tool integrated into the Tier 3 weight management service at University Hospitals Coventry and Warwickshire.
Researchers followed 412 adults with severe obesity who were referred into the service.
All were offered access to W8Buddy as part of routine care; 220 chose to use it, while 192 continued with standard clinic support only.
Participants in both groups had very high starting weights – on average around 130-134kg, with body mass index (BMI) in the high 40s.
About one in five were also living with type 2 diabetes.
Over the course of the evaluation, people using W8Buddy lost more weight than those receiving usual care alone.
Using a typical example, the authors estimated that a man starting at 130kg who stayed in the service for a year would fall to around 120kg if he used W8Buddy, compared with about 127kg with standard care only.
That equates to roughly 7-8% weight loss with the app, versus 2-3% without it.
The pattern was clear: among W8Buddy users, the longer someone stayed in the service and continued to use the tool, the more weight they tended to lose. Time in the service made little difference for non-users.
For patients with type 2 diabetes, the study also looked at changes in HbA1c, a marker of long-term blood sugar levels.
In W8Buddy users with paired results, average HbA1c fell from 59.8 mmol/mol to 51.2 mmol/mol over about nine months – a drop of roughly 8-9 mmol/mol.
Non-users with diabetes saw a smaller improvement, from 62.5 mmol/mol to 60 mmol/mol over a slightly longer period.
The study did not collect detailed data on diabetes medications, so it cannot say how much of this change was due to the app rather than drug treatment.
However, the authors note that the larger fall in HbA1c was seen in the group using the digital tool.
Beyond weight and blood sugar, the evaluation reported changes in how people felt and functioned day to day.
Among W8Buddy users who completed in-app questionnaires:
- Satisfaction with life scores rose from an average of 19.5 to 23.0 on a standardised scale – an increase of 18%.
- Daytime sleepiness scores, measured using the Karolinska Sleepiness Scale, fell from 3.9 to 3.2, suggesting people felt less drowsy.
- Self-rated health on the EQ-5D visual analogue scale improved from 60.4 to 72.0 out of 100 – a gain of 11.6 points.
Measures of depressive symptoms and the EQ-5D health index remained largely unchanged over the follow-up period, indicating the tool did not significantly shift underlying mood scores within the timeframe observed, but was associated with people feeling more satisfied with life and reporting better overall health and energy.
Engagement levels were relatively high for a real-world obesity service.
- W8Buddy app paves the way for enhanced weight management in the NHS
- Diabetes management among older people can be improved by digital apps
- Regular phone support helps weight loss patients stay on track
By the end of 2023, 1,170 patients had been told about W8Buddy and 392 (around one-third) had activated it. Of those, 83% had logged in and entered data in the previous 28 days, and just over half had completed at least 12 of the 16 education modules available.
As an observational service evaluation rather than a randomised trial, the study cannot prove that W8Buddy itself caused the improvements seen.
People who chose to use the app may have been more motivated or more ready to change than those who did not, and medication changes were not tracked.
Even so, the authors argue that the findings provide real-world evidence that a digital tool integrated into a specialist NHS obesity service can enhance outcomes.
They note that traditional Tier 3 programmes often see modest weight loss alongside high dropout, and suggest that tools like W8Buddy may offer one way to extend support and maintain progress between clinic visits.
They call for longer-term follow-up to see whether the weight, blood sugar and wellbeing improvements are sustained, and for further work to evaluate cost-effectiveness and identify which elements of the digital support are most important for patients.