- Researchers identified a potentially protective type of immune cell in fat tissue that may help suppress inflammation linked to insulin resistance.
- In preclinical work, excess visceral fat was associated with a drop in a protein called SerpinB2, fewer protective “resident macrophages”, and worsening metabolic health.
- The findings are early-stage, but they hint at a future treatment approach that targets inflammation in fat tissue, possibly alongside GLP-1 medicines.
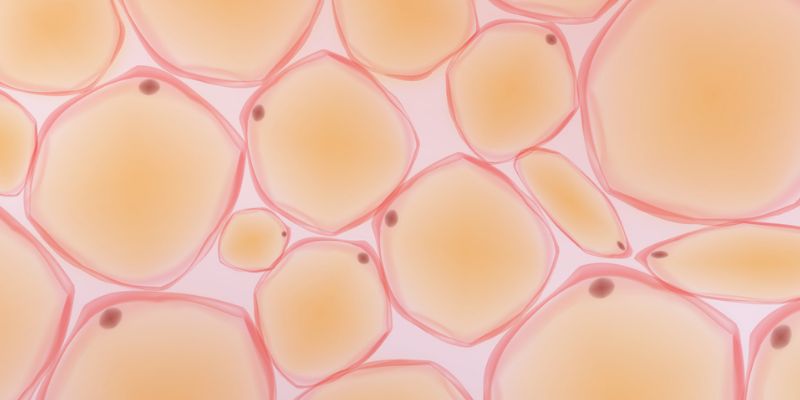
Visceral fat is the fat stored deep in the abdomen around internal organs.
It is strongly linked to inflammation and to higher risk of insulin resistance and type 2 diabetes.
Inflammation in fat tissue is not just a side effect – it can actively drive metabolic problems.
For years, scientists have tried to understand why some fat becomes more inflammatory and harmful.
In this research, scientists focused on immune cells in fat tissue called macrophages.
Macrophages can promote inflammation, but some macrophage types may do the opposite.
The team described a subset called tissue-resident macrophages.
These cells help clear dead cells, support tissue health, and may suppress the inflammatory signals that worsen insulin resistance.
A key protein in this story is SerpinB2.
The researchers reported that SerpinB2 supports the survival of these resident macrophages in chronic inflammation.
When visceral fat builds up, inflammatory stress rises and SerpinB2 levels fall.
As SerpinB2 drops, resident macrophages die off, removing a brake on inflammation.
The result is a vicious cycle.
More inflammation leads to worse insulin sensitivity, which can contribute to rising blood glucose and progression towards diabetes.
The study included experiments in mice, alongside work using human tissue.
Because much of the mechanistic work was in animals, it is best viewed as preclinical evidence, not a proven treatment pathway yet.
In the mouse model, the team tested antioxidant supplementation.
They reported an increase in resident macrophages and an improvement in insulin sensitivity in overweight mice with insulin resistance.
The researchers are now aiming to translate this into a medication strategy for humans.
They described plans to identify a small molecule that can raise SerpinB2 levels, with the goal of supporting resident macrophages and reducing harmful fat inflammation.
They also suggested this approach might complement GLP-1 treatments.
One idea is that if some people plateau on GLP-1 medicines over time, targeting fat inflammation could add another lever to improve metabolic health.
- Boosting GLP-1: how to increase GLP-1 levels naturally
- GLP1 weight loss drugs could reduce alcohol intake
- Study outlines impact of GLP-1 medications on women’s health
It is important not to over-read these findings.
Animal studies often identify promising pathways that do not translate cleanly into safe and effective human treatments.
Still, the work adds a useful piece to the bigger picture.
Type 2 diabetes risk is shaped not only by weight, but by how fat tissue behaves and how inflamed it becomes.
Study reference: Nature Communications (2026), “Tissue-resident macrophage survival depends on mitochondrial function regulated by SerpinB2 in chronic inflammation”, DOI: 10.1038/s41467-026-69196-4.