Diabetic retinopathy is the most common form of diabetic eye disease. It usually only affects people who have had diabetes (diagnosed or undiagnosed) for a significant number of years.
Retinopathy can affect all people living with diabetes and becomes particularly dangerous the longer it is left untreated, eventually resulting in blindness.
The risk of developing diabetic retinopathy is known to increase as you get older. Like other diabetes-related complications, the risk of developing the condition also increases if you do not manage your blood glucose levels sufficiently.
Diabetic Retinopathy in the UK
Of an estimated 1.93 million people living with sight loss in the UK, 4% of them are people with diabetic retinopathy.[1]
A report by the Royal National Institute of Blind people found that in 2014, the prevalence of diabetic retinopathy was 54.6% in people living with type 1 diabetes and 30% in people with type 2 diabetes. [2]
All people with diabetes should undergo an annual retinal screening appointment to spot the signs of diabetic retinopathy early on.
What is diabetic retinopathy?
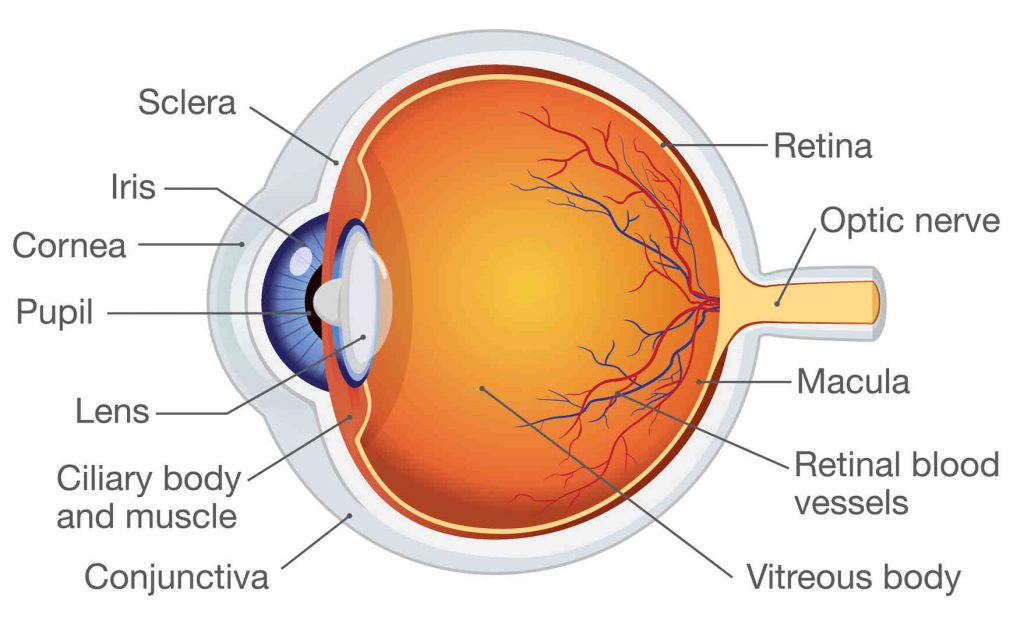
Diabetic retinopathy occurs when raised blood glucose levels cause adverse changes to retinal blood vessels to leak, grow incorrectly or become blocked.
If they swell up (macular oedema) fluid can leak into the rear of the eye. In other cases, blood vessels grow abnormally on the retina’s surface.
Unless treated, diabetic retinopathy can gradually become more serious and progress from ‘background retinopathy’ to seriously affecting vision and eventually leading to blindness.
Background retinopathy
Background retinopathy, also known as simple retinopathy, involves tiny swellings in the walls of the blood vessels. Known as blebs, they appear as small dots on the retina and are usually accompanied by yellow patches of exudates (blood proteins).
Background diabetic retinopathy requires monitoring by an ophthalmologist, so it is important to attend regular retinopathy screening appointments.
Diabetic maculopathy
The macula is the most used area of the retina and provides us with our central vision. Diabetic maculopathy refers to a progression of background retinopathy into the macula.
This can cause vision problems such as difficulty with reading and or seeing faces in the centre of your vision.
Proliferative retinopathy
Proliferative retinopathy is an advanced stage of diabetic retinopathy in which the retina becomes blocked causing the growth of abnormal blood vessels. These blood vessels can bleed into the eyes, causing the retina to become detached and serious vision damage.
Left untreated, this can eventually lead to blindness. If proliferative retinopathy is regularly monitored and treated, the development of retinopathy can be limited, preventing more severe damage.
What are the symptoms of diabetic retinopathy?
Like many conditions of this nature, the early stages of diabetic retinopathy can occur without any initial symptoms and without pain. A noticeable effect on the vision does not typically occur until the disease advances.
Symptoms might only be identified once the disease advances, but the typical symptoms of retinopathy to look out for include:
- Sudden changes in vision / blurred vision
- Eye floaters and spots
- Double vision
- Eye pain
You can read more about the symptoms of diabetic retinopathy here.
If you are experiencing any of the symptoms of diabetic retinopathy, don’t wait until your next eye screening to talk to your healthcare professional. Seek advice from your GP or other healthcare professional as soon as possible.
What causes diabetic retinopathy?
Diabetic retinopathy is caused by having high blood glucose levels for long periods of time. Prolonged bouts of high sugar glucose levels can weaken and damage the small blood vessels within the retina. This may cause haemorrhages, exudates and even swelling of the retina. Over time, the retina eventually becomes starved of oxygen and abnormal blood vessels start to grow.
Good blood glucose control helps to lower diabetic retinopathy risks.
Am I at risk from diabetic retinopathy?
Diabetic retinopathy risk factors include the following.
- Poor blood glucose control
- Protein in urine
- High blood pressure
- Prolonged diabetes
- Raised fats (triglycerides) in the blood
Anyone suffering from diabetes faces the risk of developing diabetic retinopathy and other diabetes complications.
The longer a person has diabetes, the greater the risk of developing diabetic retinopathy becomes. However, keeping blood glucose levels well controlled can help to slow down the development of retinopathy significantly.
Be aware that a rapid improvement in blood glucose levels – defined as a drop in HbA1c of 30mmol/mol or 3% – can actually lead to a worsening of retinopathy.
Are there any ways to prevent diabetic retinopathy?
Long-term good blood glucose level management helps to prevent diabetes retinopathy and lower the risk of developing it.
The risk of developing diabetic retinopathy can be lessened through taking the following precautions:
- Having a dilated eye examination at least once a year.
- Strictly managing diabetes through medicine, insulin, diet and exercise
- Frequently testing blood sugar levels.
- Regularly testing urine for ketone levels.
Can diabetic retinopathy be treated?
Laser surgery is often used in the treatment of diabetic eye disease, but each stage of diabetic retinopathy can be treated in a different way.
Background retinopathy has no treatment but patients will need to have regular eye examinations.
Maculopathy is usually treated with laser treatment, (tiny burns that help to prevent new blood vessel growth and improve the nutrient and oxygen supply to the retina). This is usually painless and has no side effects, but can influence night driving and peripheral vision.
This type of laser treatment for diabetic retinopathy will not improve vision, but it can prevent deterioration. Proliferative retinopathy is also treated with lasers, with a scattering over the whole retina. This destroys the starved area of the retina.
Serious diabetes retinopathy cases may require eye surgery.
This is usually diagnosed due to bleeding in the eye, late-stage proliferative retinopathy or ineffective laser treatment. This type of diabetic retinopathy eye surgery is called vitrectomy.
- Read more about treating retinopathy.
What members of the Diabetes Community are saying about diabetic eye disease:
- “Hi I’m type 1 diabetic and have been for nearly 22 years. I’m also 24 weeks pregnant and I’ve had my diabetic eye screening recently and its come back saying I have got diabetes maculopathy…”
- “… I had my first retinopathy screening and got the results today and I have maculopathy. I have been referred to the eye hospital for assessment. Right now I am terrified…”
- “Following eye test last week, I’ve just received letter saying I have background retinopathy in right eye. I feel sick with worry. I had a baby last year and heard eye sight can worsen. My hba1c has been normal since diagnosis 2 years ago with latest 36. But I do have occasional highs…”